Prof. James de Lemos (University of Texas Southwestern Medical Center, USA) explained the main objectives of the registry: 1) to accelerate the pace of COVID-19 research and improve quality, in view of the unprecedented time horizon and the need for ‘out-of the-box’ thinking for solutions; 2) to collect granular data, with over 200 unique data elements and extensive serial laboratory data; and 3) to complete case capture from the beginning of the pandemic in order to minimise selection bias and enhance generalisability. Considering the immediate need for data, the research process was disrupted and democratised, establishing a secure cloud-based environment called the AHA Precision Medicine Platform (PMP). A novel strategy for 'burst science' that has been implemented allows multiple groups of investigators to work simultaneously on the PMP using de-identified data, in the hope that the 'door-to-dissemination' time be markedly accelerated. As of 9 November 2020, records of over 22,500 patients from 109 hospitals were available.
Prof. de Lemos showed that the majority of the 14,889 patients hospitalised for COVID-19 (data cut-off: 22 July 2020) had CV risk factors, including hypertension (58%), obesity (43%), diabetes (36%), and hyperlipidaemia (34%). Prevalent disease was also common, particularly prior chronic kidney disease or end-stage renal disease (13%), HF (11%), and prior stroke (10%). In-hospital cardiac complications were less frequent than initially anticipated. The composite CVD endpoint of CV death, MI, stroke, HF, and shock was reached by 8.8% of hospitalised patients. Looking at individual complications, AF was reported in 8.0%, deep vein thrombosis/pulmonary embolism in 3.8% (substantially less than reported in single-centre experiences), MI in 2.5%, stroke, new HF, and cardiogenic or mixed shock in <2%, and myocarditis in 0.3%. Death occurred in 16.7% of patients (10% had a CV cause), with another 2.8% referred to hospice. Non-cardiac complications included ICU admission in 30%, mechanical ventilation in 20%, and new dialysis/CRRT in 4.0%.
“The COVID-19 pandemic has driven disruptive –and we believe enduring– innovation to registry research,” Prof. de Lemos concluded. “COVID-19 admissions have a high prevalence of CVD risk factors and a moderately high prevalence of prior CVD. Unfortunately, the pandemic has a depressingly high mortality and morbidity rate. CV complications are an important subset but are less common than initially feared. Given the scale of the pandemic, with currently almost 70,000 COVID-19 patients hospitalised in the US, the cumulative number of these CV events is still large.”
- De Lemos JA, et al. The AHA COVID-19 Cardiovascular Disease Registry: Design, Implementation, and Initial Results. 08, AHA Scientific Sessions 2020, 13–17 Nov.
Posted on
Previous Article
« ASCO GU 2021 Highlights Podcast Next Article
AF screening in older adults at primary care visits »
« ASCO GU 2021 Highlights Podcast Next Article
AF screening in older adults at primary care visits »
Table of Contents: AHA 2020
Featured articles
COVID-19 and Influenza
Fewer CV complications than expected in AHA COVID-19 Registry
Worse COVID-19 outcomes in younger obese patients
Effects of CVD in hospitalised COVID-19 patients
Unfavourable outcomes for COVID-19 patients with AF and atrial flutter
High-dose influenza vaccine in patients with CVD
Atrial Fibrillation
Vitamin D or omega 3 fatty acids do not prevent AF
Active screening for AF improves clinical outcomes
AF screening in older adults at primary care visits
CVD Risk Reduction
Clever trial design gets patients back on statins: the SAMSON trial
Polypill plus aspirin reduces cardiovascular events
Lowering LDL cholesterol in older patients is beneficial
No CV benefit from omega 3 in high-risk patients
Safety and efficacy of inclisiran for hypercholesterolemia
Remote risk management programme effective and efficient
Healthy lifestyle lowers mortality irrespective of medication burden
Heart Failure
Omecamtiv mecarbil improves outcomes in HFrEF-patients
IV iron reduces HF hospitalisation
Dapagliflozin reduces renal risk independent of CV disease status
“Strongly consider an SGLT2-inhibitor in most T2DM patients”
Additional HFrEF education and patient-engagement tools
Acute Coronary Syndrome
No benefit from omega-3 fatty acids after recent MI
PIONEER III trial: Drug-eluting stents comparable
Coronary and Valve Disease
Extra imaging reveals cause of MINOCA in women
Ticagrelor not superior to clopidogrel after elective PCI
Stroke
Ticagrelor/aspirin reduces stroke risk in patients with ipsilateral cervicocranial plaque
AF monitoring following cardiovascular surgery
Miscellaneous
PAD: Rivaroxaban reduces VTE risk after revascularisation
Sotatercept: potential new treatment option for PAH
Finerenone lowers CV events in diabetic CKD patients
Mavacamten effective in obstructive hypertrophic cardiomyopathy
Children exposed to tobacco smoke have worse heart function as adults
Transgender people have unaddressed heart disease risks
Intensive blood pressure lowering benefits older adults
Longer chest compression pause worsens outcomes after paediatric IHCA
Related Articles

February 17, 2021
Unfavourable outcomes for COVID-19 patients with AF and atrial flutter
February 18, 2021
Intensive blood pressure lowering benefits older adults
February 18, 2021
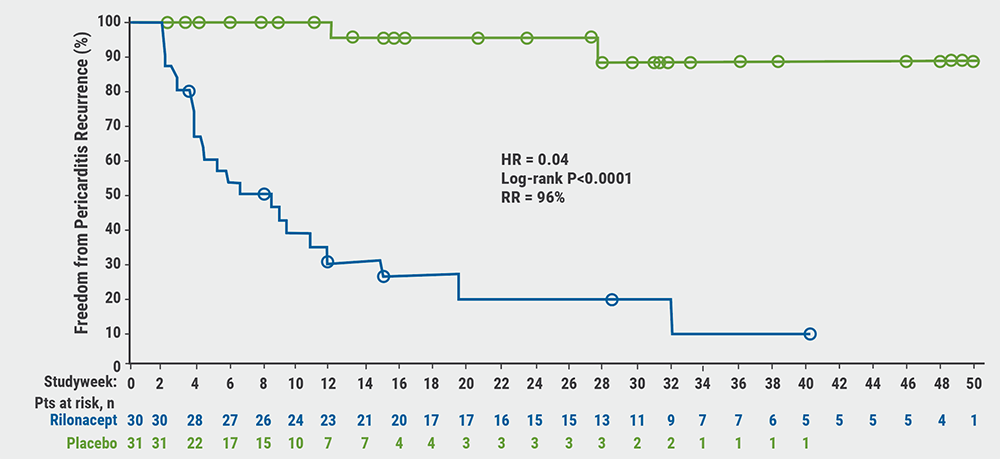
Rilonacept reduces risk of pericarditis recurrence
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

