The current analysis utilised electronic health records from 54 health systems that use a COVID-19 database. Prof. Ann Marie Navar (University of Texas Southwestern, USA) sought to understand who is most at risk, which is especially important for deploying immunisation strategies. Overall, 28,299 hospitalised patients with COVID-19 were identified. The analysis focused on 19,584 hospitalised patients who were discharged home or died in the hospital as of 1 July 2020. The median age was 52 years, 52.3% were male, 29.4% were Hispanic, and 21.5% were Black. Comorbidities were common: 50.4% had hypertension, 31.1% had diabetes, 18.0% had coronary artery disease, 14.3% had prior heart failure, and 5.6% had end-stage renal disease (see Table).
Table: Characteristics and in-hospital mortality of patients hospitalised with COVID-19 [1]

The overall in-hospital mortality was 20.7%, rising non-linearly with age, with a sharp increase above age ~60 years (P<0.0001). Female sex, white race, and Hispanic ethnicity were associated with a lower risk of death (P<0.0001 for all). On the other hand, in patients needing mechanical ventilation (32.6%), mortality was much higher: 74.6%. Mortality rates were also higher for patients with CVD (28.8%) or CVD risk factors: hypertension (mortality 20.4%), diabetes (21.5%), and heart failure (34.2%) (P<0.0001 for all). Cardiovascular complications were uncommon: myocardial infarction 5%, pulmonary embolism 2%, and stroke 1.5%. However, they were strongly associated with increased mortality risk: 55.5%, 26.5%, and 56%, respectively. Prof. Navar also observed a significant linear increase in risk of death with a decrease in BMI. “Once hospitalised, being underweight may be as much or worse of a risk factor than being overweight.”
In a multivariable analysis looking at comorbidities, BMI, and race/ethnicity, these were the main predictors of mortality:
- male sex: OR 1.46 (95% CI 1.31–1.62);
- Hispanic ethnicity: OR 0.71 (95% CI 0.59–0.86)
- diabetes: OR 1.27 (95% CI 1.13–1.42);
- heart failure: OR 1.29 (95% CI 1.13–1.47);
- chronic kidney disease: OR 1.50 (95% CI 1.32–1.69).
Prof. Navar said there is a “remarkably high risk” of death in the ~16 million Americans >80 years old with diabetes and/or hypertension when infected with COVID-19. “It seems almost impossible, then, to be advocating a strategy of focused protection or herd immunity as some in the US administration are calling for.”
- Navar A, et al. Impact of Cardiovascular Disease on Outcomes Among Hospitalized COVID-19 Patients: Results From >14,000 Patients Across the United States. LBS.08, AHA Scientific Sessions 2020, 13–17 Nov.
Posted on
Previous Article
« Meta-analyses: ACEI/ARB and COVID-19 Next Article
Worse COVID-19 outcomes in younger obese patients »
« Meta-analyses: ACEI/ARB and COVID-19 Next Article
Worse COVID-19 outcomes in younger obese patients »
Table of Contents: AHA 2020
Featured articles
COVID-19 and Influenza
Fewer CV complications than expected in AHA COVID-19 Registry
Worse COVID-19 outcomes in younger obese patients
Effects of CVD in hospitalised COVID-19 patients
Unfavourable outcomes for COVID-19 patients with AF and atrial flutter
High-dose influenza vaccine in patients with CVD
Atrial Fibrillation
Vitamin D or omega 3 fatty acids do not prevent AF
Active screening for AF improves clinical outcomes
AF screening in older adults at primary care visits
CVD Risk Reduction
Clever trial design gets patients back on statins: the SAMSON trial
Polypill plus aspirin reduces cardiovascular events
Lowering LDL cholesterol in older patients is beneficial
No CV benefit from omega 3 in high-risk patients
Safety and efficacy of inclisiran for hypercholesterolemia
Remote risk management programme effective and efficient
Healthy lifestyle lowers mortality irrespective of medication burden
Heart Failure
Omecamtiv mecarbil improves outcomes in HFrEF-patients
IV iron reduces HF hospitalisation
Dapagliflozin reduces renal risk independent of CV disease status
“Strongly consider an SGLT2-inhibitor in most T2DM patients”
Additional HFrEF education and patient-engagement tools
Acute Coronary Syndrome
No benefit from omega-3 fatty acids after recent MI
PIONEER III trial: Drug-eluting stents comparable
Coronary and Valve Disease
Extra imaging reveals cause of MINOCA in women
Ticagrelor not superior to clopidogrel after elective PCI
Stroke
Ticagrelor/aspirin reduces stroke risk in patients with ipsilateral cervicocranial plaque
AF monitoring following cardiovascular surgery
Miscellaneous
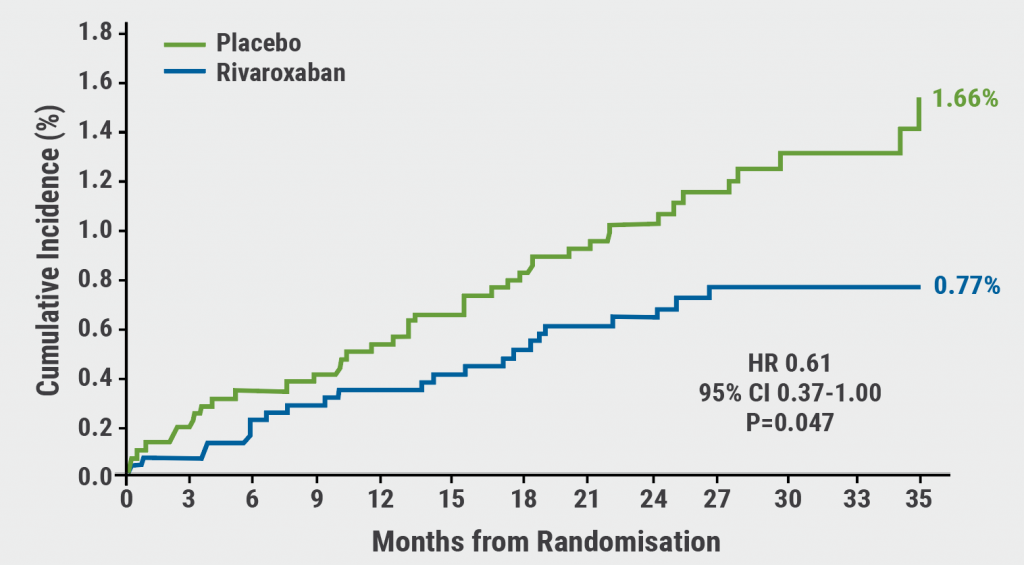
PAD: Rivaroxaban reduces VTE risk after revascularisation
Sotatercept: potential new treatment option for PAH
Finerenone lowers CV events in diabetic CKD patients
Mavacamten effective in obstructive hypertrophic cardiomyopathy
Children exposed to tobacco smoke have worse heart function as adults
Transgender people have unaddressed heart disease risks
Intensive blood pressure lowering benefits older adults
Longer chest compression pause worsens outcomes after paediatric IHCA
Related Articles
February 18, 2021
AF monitoring following cardiovascular surgery
February 18, 2021
PAD: Rivaroxaban reduces VTE risk after revascularisation
February 17, 2021
AF screening in older adults at primary care visits
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

