COVID‐19 can infect host cells through interaction with membrane‐bound ACE2 on respiratory epithelium. Theoretically, the use of ACEI and ARB may modify susceptibility to COVID-19-infection since these drugs both increase the expression of ACE. The results of 2 new meta-analyses among ACEI and/or ARB users were presented, investigating the rate of testing positive for COVID-19 and the in-hospital mortality rate for patients with COVID-19, respectively.
The first analysis included 3 studies and demonstrated that the rates of positive testing were similar for ACEI users and non-users: OR 0.96 (95% CI 0.88–1.04; P=0.69), as well as for ARB users and non-users: OR 0.99 (95% CI 0.91–1.08; P=0.35).
The second analysis included 14 studies. The results demonstrated that in-hospital mortality for patients with COVID-19 was similar between ACEI and/or ARB users and non-users: HR 0.88 (95% CI 0.64–1.20; P=0.42). A subanalysis of studies confined to patients with hypertension showed that ACEI and/or ARB use was associated with a significantly lower in-hospital mortality: HR 0.65 (95% CI 0.48–0.87).
- Yokoyama Y, et al. Meta-analyses for the Effect of Renin-angiotensin-aldosterone System Inhibitors on Mortality and Testing Positive of Covid-19. Abstract 399, AHA Scientific Sessions 2020, 13–17 Nov.
Posted on
Previous Article
« Unfavourable outcomes for COVID-19 patients with AF and atrial flutter Next Article
Effects of CVD in hospitalised COVID-19 patients »
« Unfavourable outcomes for COVID-19 patients with AF and atrial flutter Next Article
Effects of CVD in hospitalised COVID-19 patients »
Table of Contents: AHA 2020
Featured articles
COVID-19 and Influenza
Fewer CV complications than expected in AHA COVID-19 Registry
Worse COVID-19 outcomes in younger obese patients
Effects of CVD in hospitalised COVID-19 patients
Unfavourable outcomes for COVID-19 patients with AF and atrial flutter
High-dose influenza vaccine in patients with CVD
Atrial Fibrillation
Vitamin D or omega 3 fatty acids do not prevent AF
Active screening for AF improves clinical outcomes
AF screening in older adults at primary care visits
CVD Risk Reduction
Clever trial design gets patients back on statins: the SAMSON trial
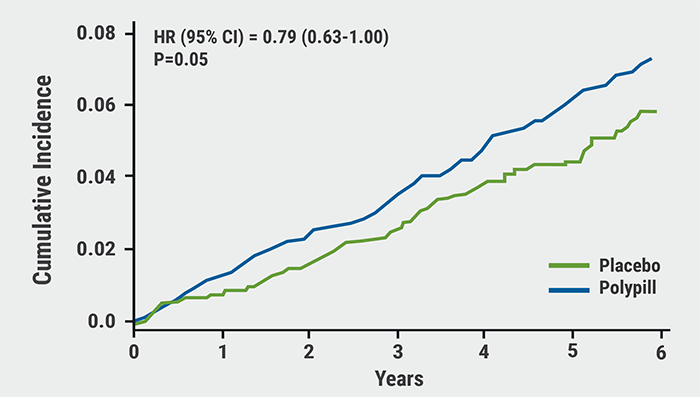
Polypill plus aspirin reduces cardiovascular events
Lowering LDL cholesterol in older patients is beneficial
No CV benefit from omega 3 in high-risk patients
Safety and efficacy of inclisiran for hypercholesterolemia
Remote risk management programme effective and efficient
Healthy lifestyle lowers mortality irrespective of medication burden
Heart Failure
Omecamtiv mecarbil improves outcomes in HFrEF-patients
IV iron reduces HF hospitalisation
Dapagliflozin reduces renal risk independent of CV disease status
“Strongly consider an SGLT2-inhibitor in most T2DM patients”
Additional HFrEF education and patient-engagement tools
Acute Coronary Syndrome
No benefit from omega-3 fatty acids after recent MI
PIONEER III trial: Drug-eluting stents comparable
Coronary and Valve Disease
Extra imaging reveals cause of MINOCA in women
Ticagrelor not superior to clopidogrel after elective PCI
Stroke
Ticagrelor/aspirin reduces stroke risk in patients with ipsilateral cervicocranial plaque
AF monitoring following cardiovascular surgery
Miscellaneous
PAD: Rivaroxaban reduces VTE risk after revascularisation
Sotatercept: potential new treatment option for PAH
Finerenone lowers CV events in diabetic CKD patients
Mavacamten effective in obstructive hypertrophic cardiomyopathy
Children exposed to tobacco smoke have worse heart function as adults
Transgender people have unaddressed heart disease risks
Intensive blood pressure lowering benefits older adults
Longer chest compression pause worsens outcomes after paediatric IHCA
Related Articles
February 17, 2021
Meta-analyses: ACEI/ARB and COVID-19
February 17, 2021
Polypill plus aspirin reduces cardiovascular events
February 18, 2021
Dobutamine versus milrinone in cardiogenic shock
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

