In 2015, the International Association for the Study of Lung Cancer Lung Cancer Staging Project made some proposals for the revision of the TNM classification for lung cancer [1]. “It was acknowledged that the amount of nodal disease has a prognostic impact”, Dr Ramón Rami-Porta (Hospital Universitari MútuaTerrassa, Barcelona, Spain) said during the first lecture. If the tumour is confined to a single station (cN2), some surgeons promote upfront resection. Furthermore, determination of the prognosis has been refined and stratification for future trials has improved.
In the revised 8th edition of the TNM classification for lung cancer [2], additional T categories based on size were described. “Perhaps pN2a1 could be considered a subgroup of early disease”, Dr Rami-Porta suggested. “Currently, we can better stratify tumours based on anatomic extent. Finally, in the revised edition of this classification system, there is the possibility to combine factors in prognostic groups.”
Is invasive staging necessary?
The question is if invasive staging is necessary in early stage non-small cell lung cancer (NSCLC). “This is not a new question”, said Dr Weder, reflecting on the title of his lecture. “Since the introduction of the PET scan, this topic has been discussed. The answer depends on the situation.”
Images of CT and PET-CT scans provide relevant information. However, in up to 20% of cases, unforeseen pN2 is present. Staging of the mediastinum begins with imaging using CT, PET-CT, or eventually MRI. “Afterwards, we decide if a tissue sample is needed”, Dr Weder continued.
The negative predictive value (NPV) of PET and CT for determining mediastinal metastasis in early stage (T1-2N0) NSCLC has been studied extensively. A meta-analysis, which evaluated 10 studies with 1,122 patients totally, showed an NPV of 94% in case of small tumours (T1; ≤3 cm) and an NPV of 89% in case of larger tumours (T2; >3 cm) [3].
Invasive staging
Techniques for invasive non-surgical staging include endobronchial ultrasound-guided biopsy (EBUS-TBNA) and endoscopic ultrasound-guided fine needle aspiration (EUS-FNA). Techniques for invasive surgical staging include cervical mediastinoscopy, eventually anterior mediastinotomy in case of a very large tumour or lymph node, and video-assisted thoracoscopic surgery (VATS), which is used more often currently.
In the beginning of this millennium, the role of extended mediastinoscopies, called video-assisted mediastinoscopic lymphadenectomy (VAMLA) and transcervical extended mediastinal lymphadenectomy (TEMLA), was studied [4]. “However, this technique is so far only applied in very selected, experienced centers”, Dr Weder added. The accuracy is high, but there is higher morbidity and mortality. So, it is not recommended for routine use.
- Asamura H, et al. J Thorac Oncol. 2015;10:1675-84.
- Goldstraw P, et al. J Thorac Oncol. 2016;11:39-51.
- Wang J, et al. Clin Lung Cancer. 2012;13:81-9.
- Hürtgen M, et al. Eur J Cardiothorac Surg. 2002;21:348-51.
Posted on
Previous Article
« Combo I-O plus chemotherapy Next Article
Incidence and local treatment »
« Combo I-O plus chemotherapy Next Article
Incidence and local treatment »
Table of Contents: ELCC 2019
Featured articles
Electromagnetic navigation bronchoscopy
Current Management of Early Stage NSCLC
Trial Data: Early Stage Lung Cancer
Electromagnetic navigation bronchoscopy
Genomic and immune profiling
Immunotherapy in Stage 4 Lung Cancer
Other I-O combinations
Predictive diagnostics for I-O
Trials: Immunotherapy in Stage 4 Lung Cancer
Post-study immunotherapy in MYSTIC
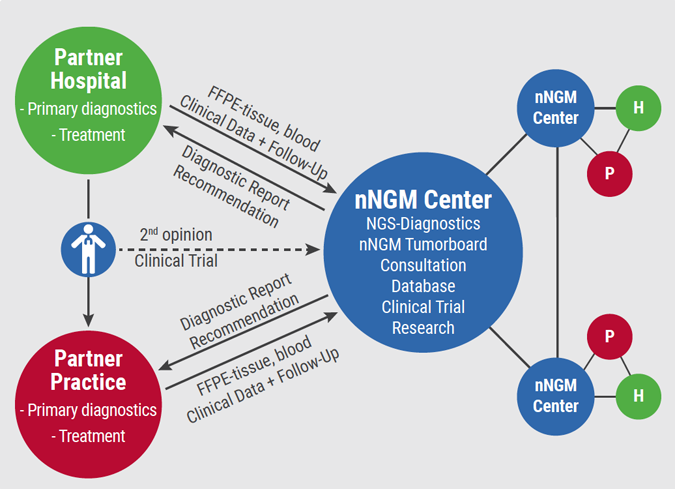
Implementation of Personalised Lung Cancer Care in Clinical Routine
How can societies help to implement personalised treatment?
Optimal Management of Brain Metastases in NSCLC
Incidence and local treatment
Brain irradiation as treatment option
Small Cell Lung Cancer: New Targets
Molecular characteristics of SCLC
Immunotherapy in SCLC: trial data
Related Articles
June 25, 2019
Combo I-O plus chemotherapy
June 25, 2019
Experiences from Germany
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

