This offers a unique opportunity to select patients for systemic therapy of this ‘sanctuary site’. In decision-making, consultation within the multidisciplinary team is essential. “We really need a team approach”, Dr Natasha Leighl (Princess Margaret Cancer Centre, Toronto, Canada) emphasised.
Sequencing systemic therapy without driver mutations
In non-oncogene-addicted NSCLC, the management of CNS metastases is harder compared with the treatment of oncogene-addicted lung cancer. Dr Leighl mentioned some key questions:
- Should we start with local or systemic therapy? Do we have to choose based on symptoms, disease burden, CNS penetration of systemic agent, or other reasons?
- If we start with systemic therapy, how often should we image? Her advice is every 8 to 12 weeks, depending on symptoms.
- If progression is restricted to the CNS, can we switch treatments to defer radiotherapy? If non-EGFR/ALK/ROS1-positive lung cancer, Dr Leighl recommends consulting a radiation oncologist.
Sequencing systemic therapy with driver mutations
The treatment paradigm of brain metastasis in oncogene-addicted lung cancer has changed dramatically, Dr Edrune Arriola Aperribay (Hospital del Mar, Barcelona, Spain) said at the beginning of her lecture. Currently, patients with molecularly driven lung adenocarcinoma are effectively treated with targeted agents. “Unfortunately, in most cases tumours will develop mechanisms of resistance, but these can be targeted in some cases with a systemic treatment [1].
Approximately 15% of NSCLC patients in Western population have an EGFR-positive tumour. They have a relatively long-term survival (>2 years) compared with EGFR-negative tumours. However, frequently (in 25% of cases), brain metastases are present at the time of diagnosis. First- and second-generation EGFR TKIs for the treatment of these patients include erlotinib, gefitinib, afatinib, and icotinib [2]. In the NCCN guidelines [3], the third generation EGFR TKI osimertinib is preferred”, Dr Arriola Aperribay added. The majority of patients with EGFR-positive NSCLC will have disease progression, most frequently in the brain. “In that scenario, we always have to evaluate the T790M mutation”, she recommends. In case of T790M-positive NSCLC, she advises to start with osimertinib, based on the results of the phase 3 AURA3 trial [4]. In this study, median CNS-related progression-free survival (PFS) was 11.7 months for patients on osimertinib compared with 5.6 months for patients on platinum- pemetrexed (HR 0.32; 95% CI 0.15-0.69; P=0.004). “These are quite interesting data for these patients.”
The phase 3 FLAURA trial compared first-line treatment with osmertinib versus gefitinib or erlotinib of patients with -positive NSCLC. A subgroup analysis showed that median CNS-related (PFS) in patients with measurable and/or non-measurable CNS lesions was not reached with osimertinib and 13.9 months with the other EGFR TKIs (HR 0.48; P=0.014) [5].
ALK-rearrangement is present in 3-5% of NSCLC patients. The incidence of brain metastases is very high in these patients: 30-40% at diagnosis and 60% during the course of the disease. Because of the introduction of many effective targeted agents in the last years, it is time to adjust current treatment algorithms [3,6,7]. Crizotinib could be used upfront, but it has a particular poor CNS penetrance [8]. Currently, drugs with a higher CNS penetrance are available. For example, the ALEX trial showed that alectinib is more effective and has lower toxicity in primary treatment of ALK-positive NSCLC compared with crizotinib [9].
More recently, another drug with very high CNS activity has become available: brigatinib. The open-label, phase 3 ALTA-1L trial showed that the rate of PFS was higher with brigatinib than with crizotinib as first-line treatment of patients with ALK-positive NSCLC (estimated 12-month PFS, 67% vs 43%; HR for disease progression or death, 0.49; P<0.001) [10]. “So, very interesting data in this setting”, according to Dr Arriola Aperribay.
- Salgia R. Expert Rev Mol Diagn. 2016;16:737-49.
- Remon J, Besse B. Front Oncol. 2018;8:88.
- Ettinger DS, et al. J Natl Compr Canc Netw. 2018;16:807-821.
- Wu YL, et al. J Clin Oncol. 2018;36:2702-2709.
- Reungwetwattana T, et al. J Clin Oncol. 2018:JCO2018783118.
- Griesinger F, et al. Oncotarget. 2018;9:35181-35194.
- Planchard D, et al. Ann Oncol. 2018;29(Supplement_4):iv192-iv237.
- Novello S, et al. Ann Oncol. 2018;29:1409-1416.
- Peters S, et al. N Engl J Med. 2017;377:829-838.
- Camidge DR, et al. N Engl J Med. 2018;379:2027-2039.
Posted on
Previous Article
« How can societies help to implement personalised treatment? Next Article
Immunotherapy in SCLC: trial data »
« How can societies help to implement personalised treatment? Next Article
Immunotherapy in SCLC: trial data »
Table of Contents: ELCC 2019
Featured articles
Electromagnetic navigation bronchoscopy
Current Management of Early Stage NSCLC
Trial Data: Early Stage Lung Cancer
Electromagnetic navigation bronchoscopy
Genomic and immune profiling
Immunotherapy in Stage 4 Lung Cancer
Other I-O combinations
Predictive diagnostics for I-O
Trials: Immunotherapy in Stage 4 Lung Cancer
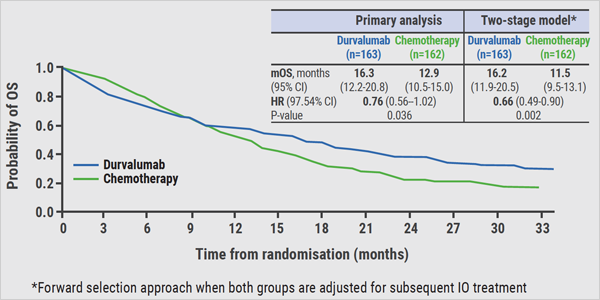
Post-study immunotherapy in MYSTIC
Implementation of Personalised Lung Cancer Care in Clinical Routine
How can societies help to implement personalised treatment?
Optimal Management of Brain Metastases in NSCLC
Incidence and local treatment
Brain irradiation as treatment option
Small Cell Lung Cancer: New Targets
Molecular characteristics of SCLC
Immunotherapy in SCLC: trial data
Related Articles
June 25, 2019
I-O monotherapy
June 25, 2019
Treatment options in early NSCLC

June 25, 2019
Letter from the editor
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

