The BMI analysis from the AHA COVID-19 CVD Registry was presented by Dr Nicholas Hendren (University of Texas Southwestern, USA). The study's hypothesis was that obesity is associated with worse outcomes in COVID-19, especially in younger patients. The primary outcome was a composite of in-hospital death or mechanical ventilation, as well as the individual components of in-hospital death and mechanical ventilation. Secondary endpoints included major adverse cardiovascular events (MACE), venous thromboembolism, and renal replacement therapy.
BMI data was available for 7,606 patients. Mean BMI in this cohort was higher than that in the US National Health and Nutrition Examination Survey (NHANES), especially among patients aged ≤50 years. In this sample, 194 patients were underweight (BMI <18.5 kg/m2), 1,793 had a normal weight (BMI 18.5–24.9 kg/m2), 2,308 had overweight (BMI 25–29.5 kg/m2), 1,623 had class I obesity (BMI 30–34.9 kg/m2), 846 had class II obesity (BMI 35–39.5 kg/m2), and 842 had class III obesity (BMI ≥40 kg/m2). Obesity was associated with an elevated risk for the primary endpoint compared with normal weight. The risk increased with worse degrees of obesity:
- class I obesity: OR 1.28 (95% CI 1.09–1.51);
- class II obesity: OR 1.57 (95% CI 1.29–1.91);
- class III obesity: OR 1.80 (95% CI 1.47–2.20).
Dr Hendren noted that the differences were mainly driven by the risk of mechanical ventilation, which was significantly higher in overweight and obese patients than in patients with normal weight.
No association was seen between obesity class and risk of MACE (i.e. all-cause death, in-hospital stroke, heart failure, or myocardial infarction). Only class II obesity was associated with a higher risk of venous thromboembolism. Obesity classes I, II, and III were associated with a stepwise increase in the risk of in-hospital initiation of renal replacement therapy. Class III obesity was associated with elevated risk of in-hospital mortality only in patients aged ≤50 years (HR 1.36; 95% CI 1.01–1.84). The risks of poor outcomes related to obesity were most pronounced in patients aged ≤50 years (P for interaction <0.05 for all primary endpoints).
“We believe that clear public health messaging is needed for younger obese individuals who may underestimate their risk if they get COVID-19,” Dr Hendren concluded. “Severely obese individuals should be considered at high risk for severe COVID-19 disease and may warrant prioritisation for a COVID-19 vaccine.”
- Hendren N, et al. Association of Body Mass Index with Death, Mechanical Ventilation, and Cardiovascular Outcomes in COVID-19: Findings from the AHA COVID-19 Cardiovascular Disease Registry. LBS.08, AHA Scientific Sessions 2020, 13–17 Nov.
- Hendren N, et al. Circulation. 2021;143:135–144.
Posted on
Previous Article
« Effects of CVD in hospitalised COVID-19 patients Next Article
ASCO GU 2021 Highlights Podcast »
« Effects of CVD in hospitalised COVID-19 patients Next Article
ASCO GU 2021 Highlights Podcast »
Table of Contents: AHA 2020
Featured articles
COVID-19 and Influenza
Fewer CV complications than expected in AHA COVID-19 Registry
Worse COVID-19 outcomes in younger obese patients
Effects of CVD in hospitalised COVID-19 patients
Unfavourable outcomes for COVID-19 patients with AF and atrial flutter
High-dose influenza vaccine in patients with CVD
Atrial Fibrillation
Vitamin D or omega 3 fatty acids do not prevent AF
Active screening for AF improves clinical outcomes
AF screening in older adults at primary care visits
CVD Risk Reduction
Clever trial design gets patients back on statins: the SAMSON trial
Polypill plus aspirin reduces cardiovascular events
Lowering LDL cholesterol in older patients is beneficial
No CV benefit from omega 3 in high-risk patients
Safety and efficacy of inclisiran for hypercholesterolemia
Remote risk management programme effective and efficient
Healthy lifestyle lowers mortality irrespective of medication burden
Heart Failure
Omecamtiv mecarbil improves outcomes in HFrEF-patients
IV iron reduces HF hospitalisation
Dapagliflozin reduces renal risk independent of CV disease status
“Strongly consider an SGLT2-inhibitor in most T2DM patients”
Additional HFrEF education and patient-engagement tools
Acute Coronary Syndrome
No benefit from omega-3 fatty acids after recent MI
PIONEER III trial: Drug-eluting stents comparable
Coronary and Valve Disease
Extra imaging reveals cause of MINOCA in women
Ticagrelor not superior to clopidogrel after elective PCI
Stroke
Ticagrelor/aspirin reduces stroke risk in patients with ipsilateral cervicocranial plaque
AF monitoring following cardiovascular surgery
Miscellaneous
PAD: Rivaroxaban reduces VTE risk after revascularisation
Sotatercept: potential new treatment option for PAH
Finerenone lowers CV events in diabetic CKD patients
Mavacamten effective in obstructive hypertrophic cardiomyopathy
Children exposed to tobacco smoke have worse heart function as adults
Transgender people have unaddressed heart disease risks
Intensive blood pressure lowering benefits older adults
Longer chest compression pause worsens outcomes after paediatric IHCA
Related Articles
February 24, 2021
Letter from the Editor
February 18, 2021
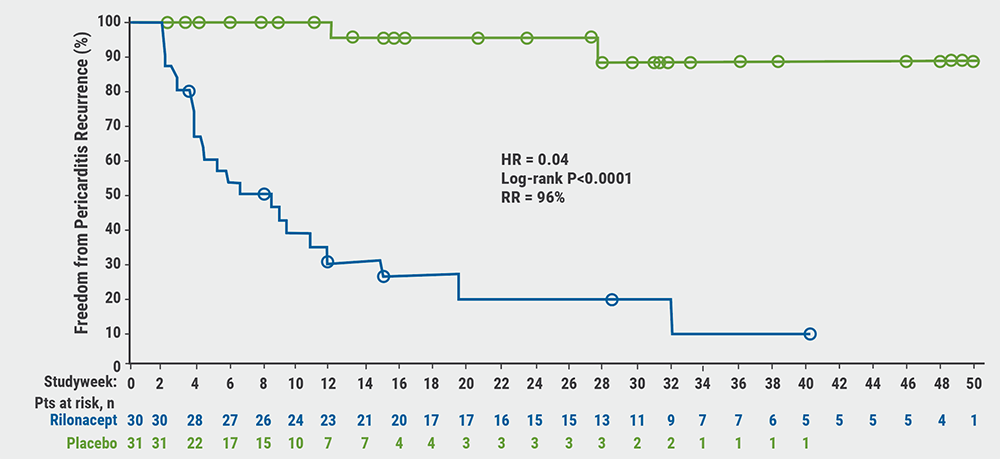
Rilonacept reduces risk of pericarditis recurrence
February 17, 2021
Vitamin D or omega 3 fatty acids do not prevent AF
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

