https://doi.org/10.55788/98db74b5
Treatment of acute ischaemic stroke (AIS) with mechanical thrombectomy is strongly time dependent and since 2018 it is mainly applied 6–30 hours after AIS. In this late time-window, patient selection is based on advanced neuroimaging, which needs to demonstrate a significant penumbra in order for a patient to be selected for thrombectomy. In the early time-window (<6 hours after AIS), there is no need for this type of advanced penumbra imaging; a CT-scan or MRI is sufficient. Dr Davide Strambo (University of Lausanne, Switzerland) and colleagues aimed to investigate whether pre-treatment perfusion parameters are associated with outcome in AIS patients treated with mechanical thrombectomy within 6 hours [1].
To this end, a retrospective, single-centre analysis based on the ASTRAL registry was performed, including AIS patients with anterior circulation large vessel occlusion (LVO), treated within 6 hours, and with available baseline perfusion data. CT and MRI data allowed for quantification of the volume of the core, i.e. tissue that is irreversibly injured, and of the penumbra, i.e. tissue at risk. Based on these data, the absence of a core/penumbra “mismatch” was assessed (according to EXTEND 1A, SWIFT/PRIME, DEFUSE 3, and DAWN trials criteria), as well as ischaemic core and penumbra volumes, and perfusion/core ratio. The primary outcome was the 3-month unfavourable shift on the modified Rankin Scale (mRS>2).
Included were 262 patients, with a mean age of 70 years and 40% were women. Median National Institutes of Health Stroke Scale (NIHSS) at admission was 16, median onset-to-imaging was 100 minutes, and median onset-to-groin was 190 minutes. Median core volume was 24.4 mL (95% CI 8.0–62.4) and median penumbra volume was 113.5 mL (95% CI 68.7–164.6). Calculating the mismatch ratio showed that 20% of patients had a penumbra/core ratio <1.2, 7% between 1.2–1.8, and 73% >1.8.
“About one third of patients lacked the favourable target mismatch according to the criteria of the EXTEND 1A, SWIFT/PRIME, and DEFUSE 3 criteria,” Dr Strambo noted. When comparing outcomes at 3 months, an unfavourable outcome was associated with a larger ischaemic core, a slightly smaller penumbra, and a lower core/penumbra ratio (see Table).
Table: Associations between perfusion parameters and unfavourable outcome at 3-months by modified Rankin Scale [1]

The absence of mismatch was independently associated with a significant shift towards worse disability at 3 months, with OR varying depending on trial criteria:
- EXTEND 1A trial: OR 2.77 (95 % CI 1.53–5.04; P=0.001);
- SWIFT/PRIME trial: OR 2.72 (95 % CI 1.54–4.81; P=0.001);
- DEFUSE-3 trial: OR 2.65 (95 % CI 1.49–4.70); P=0.001);
- DAWN trial: OR 3.26 (95 % CI 1.87–5.67; P=0.001).
- Any mismatch: OR 2.72 (95 % CI 1.45–5.07; P=0.002).
These results suggest there could be reason for a paradigm shift from time-window to tissue-window in acute stroke managements.
- Schwarz G, et al. Perfusion imaging in large vessel occlusion stroke within 6 hours from onset: from time-window to tissue window. OPR-015, EAN 2022, 25–28 April, Vienna, Austria.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Intestinal alterations in patients with Parkinson’s disease Next Article
Absence of Susceptibility Vessel Sign points to malignancy in stroke patients »
« Intestinal alterations in patients with Parkinson’s disease Next Article
Absence of Susceptibility Vessel Sign points to malignancy in stroke patients »
Table of Contents: EAN 2022
Featured articles
Letter from the Editor
Overarching Theme
Migraine
Targeting cortical activation by transcranial magnetic stimulation
Erenumab more than doubles plasma CGRP levels
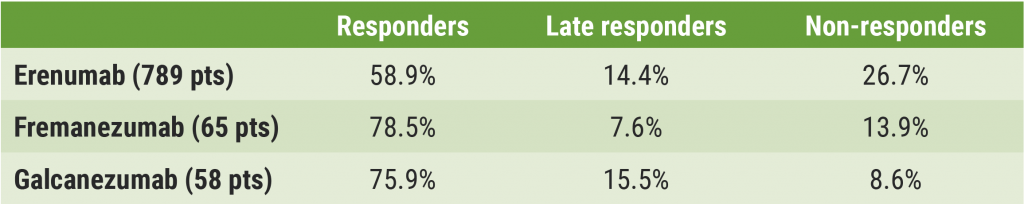
Over a third of patients responds late to CGRP antibodies
Multiple Sclerosis
When to start, switch, and stop MS therapy: Real-world evidence counts
Updated EAN-ECTRIMS guideline on pharmacological MS treatment
Gut microbiota composition associated with disability worsening
Teriflunomide in children with MS: final results of TERIKIDS
Estimating brain age in MS: machine learning versus deep learning
Ofatumumab improves cognitive processing speed
Parkinson’s Disease
Intestinal alterations in patients with Parkinson’s disease
Gene variants impact survival in monogenic Parkinson’s disease
Cerebrovascular Disease and Stroke
Most acute stroke patients have undiagnosed risk factors
Absence of Susceptibility Vessel Sign points to malignancy in stroke patients
Acute stroke management: from time window to tissue window?
Epilepsy
Seizure forecasting with non- and minimally-invasive devices
Real-world efficacy of cenobamate in focal-onset seizures
Possible new biomarker for early neuronal death in mesial temporal lobe epilepsy
COVID-19
COVID-19 elevates risk of neurodegenerative disorders
More headaches in adolescents during COVID-19 pandemic
AstraZeneca vaccination and risk of cerebral venous sinus thrombosis
Large impact of COVID-19 on dementia diagnosis and care
Miscellaneous
Tau autoimmunity associated with systemic disease
Long-term effects of avalglucosidase alfa in late-onset Pompe disease
European survey of patient satisfaction in the treatment of cancer-related neuropathic pain
Related Articles

July 14, 2022
EAN 2022 Highlights Podcast
August 22, 2022
Over a third of patients responds late to CGRP antibodies
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

