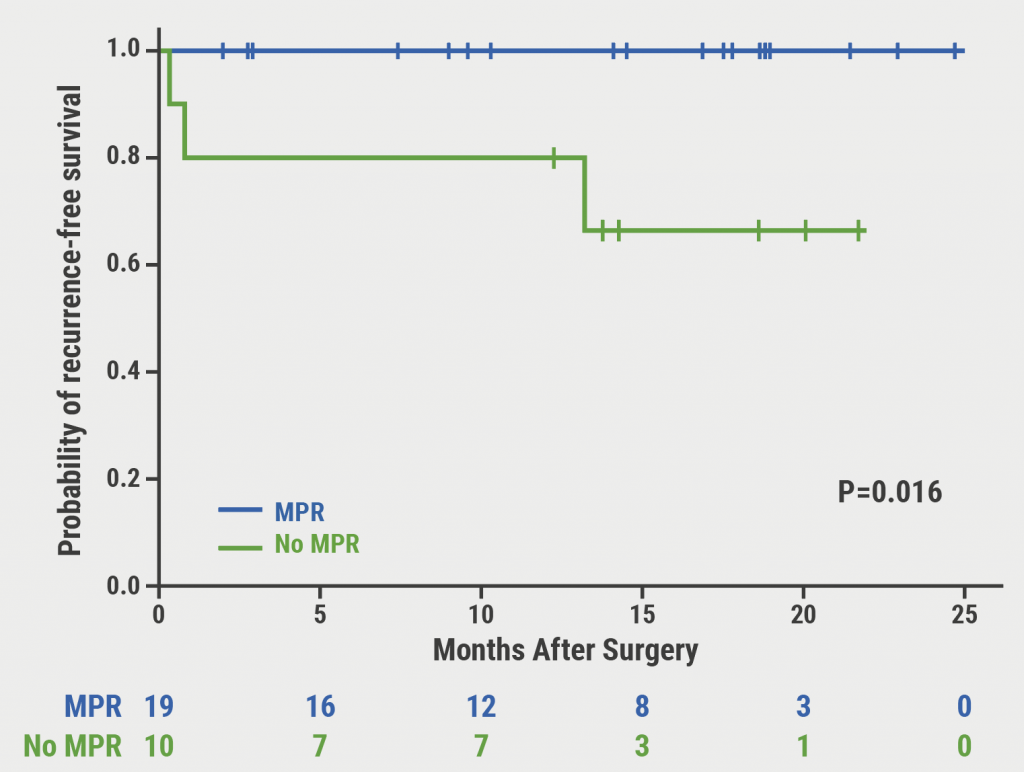
Increased cyclic adenosine monophosphate (cAMP) phosphodiesterase (PDE) activity in peripheral blood leukocytes is associated with the immune and inflammatory hyperreactivity that characterises atopic dermatitis (AD). PDE inhibitors exert an anti-inflammatory action by increasing the intracellular cAMP concentration, inhibiting the production of inflammatory cytokines (interferon-gamma, TNF-alpha, IL-4, IL-12, IL-17a, and IL-23) and other inflammatory mediators. “Difamilast is a novel hyperselective PDE-4B Blocker that looks really promising,” said Prof. David Cohen (New York University School of Medicine, USA) [1]. In animal models, PDE-4B turned out to be a key regulatory and therapeutic target to reduce inflammation [2]. In a poster presented during the AAD meeting, a 1% ointment containing difamilast demonstrated rapid itch relief with a median time to pruritus improvement of only 5.76 hours (see Figure), which was sustained at 29 days in patients with moderate-to-severe AD [3]. In addition, there was both a marked improvement in EASI score and sleep disturbance in patients treated twice daily with the ointment [3]. Another novel anti-inflammatory inhibitor of PDE-4 is crisaborole ointment (2%). Phase 3 studies in children and adults with mild-to-moderate AD have shown that crisaborole leads to clear or almost clear skin in about a third of patients [4,5]. “As in all studies with topical agents, there was also a sizeable effect of the vehicle, because AD patients have a benefit of the regular use of emollients,” said Prof. Cohen.
Figure: Median time to improvement of pruritus after treatment with difamilast. Success defined as Verbal Rating Scale (VRS) of 0 (No Itch) or 1 (Low) with ≥1-Point Reduction from Baseline [3]

Note: Subjects who achieved a success more than 8 hours after first treatment are not displayed in figure.
ITT population; subject responses. Kaplan-Meier plot.
IL-4/IL-13 blockade offers long term durable responses
The IL-4/IL-13 blocker dupilumab is at present approved for adult AD patients with moderate-to-severe disease. “I tend to warn my patients of conjunctivitis, which is the most frequent adverse event that is seen in 10-15% of patients. However, this side effect is easily manageable,” said Prof. Cohen. The responses seen with dupilumab are also durable, as demonstrated in the LIBERTY AD CHRONOS trial [6]. In this trial, dupilumab added to standard topical corticosteroid treatment for 1 year improved AD signs and symptoms, with acceptable safety.
There are also promising study results with dupilumab in adolescents, with a third obtaining almost clear skin [7]. In adolescents with severe disease, a high medical need exists for an effective treatment. “Hopefully, this study will lead to the approval of dupilumab in adolescents,” said Prof. Cohen.
Selective IL-13 blockers in the pipeline
Tralokinumab is an interesting new agent that blocks IL-13 only. In a phase 2 study, therapy with tralokinumab in combination with topical steroids led to significant reductions in S. aureus colonisation compared with topical steroids with placebo [8]. “This is an interesting study, because now we have documented that if you get greater control of the disease, you also induce a change in the microbiome,” said Prof. Cohen. This effect might potentially lead to fewer skin infections and AD flares, in addition to improving disease severity scores.
JAK inhibitors are also an interesting addition to the AD armamentarium. Baricitinib is already approved for the therapy of rheumatoid arthritis, and a phase 2 study showed that this JAK inhibitor is also efficacious in AD [9]. The agent showed rapid improvements in EASI, itch, sleep disturbance, and quality of life, with significant improvements seen as early as week 1. A big advantage of the JAK inhibitors is that they can be administered orally. In rheumatology, there have been recent concerns about potential thromboembolic risks with the two JAK inhibitors, baricitinib and tofacitinib [10]. “Right now, the adverse event profile looks good, but we will see how things develop. Thromboembolic events will be the caveat of these drugs,” concluded Prof. Cohen.
Another novel topical option is tapinarof cream. This agent demonstrated efficacy for patients with either psoriasis or AD. Its anti-inflammatory properties are mediated through activation of the aryl hydrocarbon receptor in multiple cell types. In addition, tapinarof impacts barrier gene expression in primary human keratinocytes. “In a dose-finding study it was tested in various doses and there is certainly some efficacy here,” said Prof. Cohen. All newer therapies offer the opportunity for a more targeted approach with fewer potential adverse events.
1. Cohen DE. Lecture S003, AAD Annual Meeting, 1-5 March 2019, Washington DC, USA.
2. Komatsu et al. Nat Commun. 2013;4:1684.
3. Eichenfield LF et al. ePoster No 8478, AAD Annual Meeting, 1-5 March 2019, Washington DC, USA.
4. Eichenfield LF et al. J Am Acad Dermatol 2017;77:641-9.
5. Paller A et al. J Am Acad Dermatol 2016;75:494-503.
6. Blauvelt A et al. Lancet 2017;389:2287-2303.
7. Simpson E et al. Abstract D3T01.1L, EADV Annual Meeting, 12-16 September 2018, Paris, France.
8. Guttman-Yassky et al. Abstract P0283, EADV Annual Meeting, 12-16 September 2018, Paris, France.
9. Simpson E et al. Abstract FC03.02, EADV Annual Meeting, 12-16 September 2018, Paris, France.
Posted on
Previous Article
« Novel anti-IgE drug enables durable urticaria control Next Article
Oral antibiotics for acne treatment »
« Novel anti-IgE drug enables durable urticaria control Next Article
Oral antibiotics for acne treatment »
Table of Contents: AAD 2019
Featured articles
Letter from the Editor
Interview with AAD president Prof. George J. Hruza
Late-Breakers
Secukinumab maintains improvements in psoriasis through 5 years of treatment
Bermekimab – a future treatment for atopic dermatitis?
JAK1/2 inhibitor effective in alopecia areata
Novel anti-IgE drug enables durable urticaria control
Dual IL-17A and IL-17F blocker leads to unprecedented response rates in psoriasis
Thicker AK lesions benefit from laser pretreatment with high channel density
New standardised cantharidin product against molluscum contagiosum efficacious in two phase 3 trials
Bruton’s tyrosine kinase inhibitor highly effective in pemphigus vulgaris
Serlopitant reduces pruritus associated with psoriasis
Atopic Dermatitis: Many New Therapies in the Pipeline
New and emerging atopic dermatitis therapies
Food triggers eczema – an imperturbable belief of patients
Psoriasis and Biologics: The Beat Goes On
Psoriasis and Biologics: The Beat Goes On
JAK Inhibitors: A New Frontier in Dermatology
JAK inhibitors: a new therapeutic tool for dermatologists
JAK inhibitors: a pathogenesis-directed therapy for alopecia areata
Can JAK inhibitors close the current therapeutic gap in AD?
Hair Loss: No Reason for Therapeutic Nihilism
Hair Loss: No Reason for Therapeutic Nihilism
Vitiligo: The Beginning of a New Era
Vitiligo in children
Surgical treatment for selected vitiligo cases
JAK-inhibitors: an emerging treatment option for vitiligo
What's New and Hot in Acne
Should we use more hormonal therapy?
Pearls of the Posters
Pemphigus patients prone to osteoporosis
Intralesional 5-fluorouracil induced high clearance rates in cutaneous squamous cell carcinoma
Related Articles
November 25, 2020
Adjuvant immune checkpoint inhibition after complete resection
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

