The COVID-19 in MS global data-sharing initiative is the largest international, real-world dataset of MS patients with suspected or confirmed COVID-19, including 4,646 (83.4%) confirmed cases from 32 countries [3]. Dr Steve Simpson-Yap (University of Melbourne, Australia) shared the updated results on the associations of anti-CD20 DMTs with COVID-19 severity relative to glatiramer acetate, all other pooled DMTs, and natalizumab.
Male sex, older age, progressive MS, and higher disability were associated with worse outcomes for SARS-CoV-2 infection. The use of anti-CD20 antibodies was associated with significantly worse COVID-19 outcomes. Compared to glatiramer acetate, ocrelizumab users were 1.6 (95% CI 1.06–2.43) times more likely to be hospitalised, and rituximab users were 2.4 (95% CI 1.54–3.81) times more likely to be hospitalised. Ocrelizumab and rituximab use was also associated with a 3.1 (95% CI 1.22–8.00) and 4.7 (95% CI 1.64–12.09) times higher risk of intensive care unit admission, respectively. Rituximab users were 3.6 (95% CI 1.38–9.20) times more likely to be given artificial ventilation; ocrelizumab users were 1.9 (95% CI 0.76–4.55) times more likely to require artificial ventilation. Rituximab users also had a 2.7 (95% CI 0.68–11.09) times higher risk to die, though this effect was non-significant.
The associations of ocrelizumab (n=1,100) and rituximab (n=636) with COVID-19 severity compared with other DMTs pooled (n=2,924) are shown in the Figure. Dr Simpson-Yap pointed out that all but one association are statistically significant, including the 2.4 times higher risk of death in rituximab users and a trend towards a higher risk of death in ocrelizumab users. Compared with natalizumab users, ocrelizumab and rituximab use was only associated with a higher risk of hospitalisation, intensive care unit admission, and artificial ventilation.
Figure: Associations of ocrelizumab and rituximab with Covid-19 severity versus other DMTs [1]
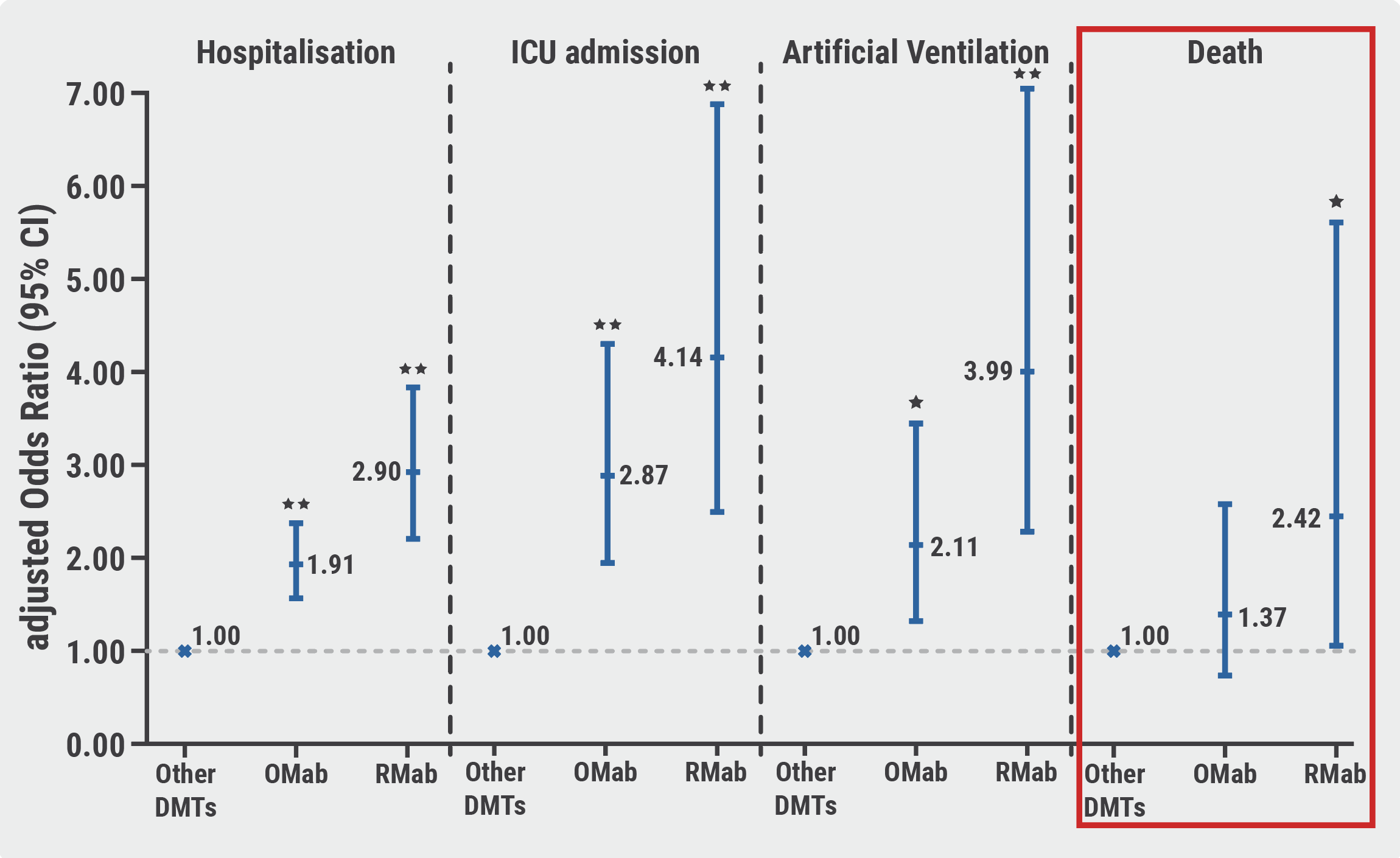 DMT, disease-modifying therapy; OMab, Ocrelizumab; RMab, rituximab. *P<0.05; **P<0.001.
DMT, disease-modifying therapy; OMab, Ocrelizumab; RMab, rituximab. *P<0.05; **P<0.001.- Simpson-Yap S, et al. Updated results of the COVID-19 in MS global data sharing initiative validate consistent associations of anti-CD20 and other reported risk factors with severe COVID-19 outcomes. OP098, ECTRIMS 2021 Virtual Congress, 13–15 October.
- Simpson-Yap S, et al. Neurology. 2021;97(19): e1870-e1885.
- Peeters LM, et al. Mult Scler. 2020;26(10):1157–1162.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« ECTRIMS-EAN consensus on vaccination in MS patients Next Article
Immunotherapy in MS does not influence COVID-19 severity and mortality »
« ECTRIMS-EAN consensus on vaccination in MS patients Next Article
Immunotherapy in MS does not influence COVID-19 severity and mortality »
Table of Contents: ECTRIMS 2021
Featured articles
Preliminary data shows positive results of ATA188 for progressive MS
COVID-19
MS patients at risk of hampered immune response after vaccination
Immunotherapy in MS does not influence COVID-19 severity and mortality
Anti-CD20 antibodies associated with worse COVID-19 outcomes
ECTRIMS-EAN consensus on vaccination in MS patients
Experimental Treatments
The role of astrocyte phenotypes in acute MS lesions
Promising results of intrathecal MSC-NTF cells in progressive MS
Preliminary data shows positive results of ATA188 for progressive MS
Evobrutinib reduces relapses and MRI lesion activity
Primary endpoint of opicinumab for relapsing MS not met in AFFINITY trial
Elezanumab did not outperform placebo in progressive and relapsing MS
Ibudilast reduced retinal atrophy in primary progressive MS
Treatment Trials and Strategies
ECTRIMS/EAN Clinical Guidelines on MS treatment: an update
Rituximab most effective initial MS therapy in Swedish real-world study
Ublituximab meets primary endpoint for relapsing MS
Dynamic scoring system aids decision to switch MS therapies early
Long-term suppression of MRI disease activity with ocrelizumab
Stopping DMT: when or if at all?
Biomarkers
Early predictors of disability progression in paediatric-onset MS
High-sensitive biomarker detection in MS via novel ELISA assay
Cortical lesions predict cognitive impairment 20 years after MS diagnosis
Applicability of sNfL measurement in clinical practice
MRI more sensitive for disease activity than relapses in SPMS
Imaging
Changes in GABA-receptor binding among cognitively impaired MS patients
T2 lesions independently predict early conversion to SPMS
Natural killer-like CD8+ T cells as a reservoir of clonal cells related to MS activity
Neuromyelitis Optica Spectrum Disorder (NMOSD)
Eculizumab, satralizumab, or inebilizumab for NMOSD?
Long-term efficacy of satralizumab for NMOSD
Long-term efficacy data: inebilizumab for NMOSD
Progressive MS
Charcot Award 2021: Progressive MS, a personal perspective
Top score poster: Meta-analysis on the effect of DMTs
Cortical lesions predict disease progression and disability accumulation
Ocrelizumab shows long-term benefits in primary progressive MS
Other
WNT9B-gene variant associated with doubled relapse risk in MS
Melatonin associated with improved sleep quality in MS patients
“Expanded Disability Status Scale 0 is not normal”
Personality trait alterations in MS patients
Related Articles
September 10, 2020
Serum NfL predicts long-term clinical outcomes in MS
December 20, 2022
New safety data of anti-CD20 mAbs around pregnancy
December 20, 2022
Study fails to show non-inferiority of rituximab to ocrelizumab
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

