Most therapeutic trials with novel agents focus on systemic lupus erythematosus (SLE) and exclude CLE patients. However, CLE and SLE share the same pathology. To solve this gap, a lupus community panel proposed to optimise future clinical trials [2]. If skin improvement is strong enough when nested in an SLE study, treatment should be made available for patients with CLE irrespective of whether they meet SLE classification. A couple of biologics have shown activity in CLE, including the IL-12/IL-23 inhibitor ustekinumab. Ustekinumab was shown to result in significant improvement in disease activity, assessed in the responder index 4 in the SLE disease activity index 2000 (SLEDAI-2K) [3].
B cells: an important novel target
The hallmark of lupus is dysregulation of B cells. B-cell-targeted therapies are therefore the focus of recent clinical research. Biologics targeting B cells are belimumab and rituximab. Belimumab is an antibody binding to the B lymphocyte stimulator (BLys), a factor involved in the survival or differentiation of B cells. The agent has shown to improve overall SLE disease activity in the most common musculoskeletal and mucocutaneous organ domains [4]. The chimeric anti-CD20 monoclonal antibody rituximab has been used with success in recalcitrant lupus manifestations [5].
Another approach: JAK inhibitors and IFNAR antibodies
First data from a double-blind, placebo-controlled, phase 2 trial with the Janus Kinase (JAK)1 and JAK2 inhibitor baricitinib showed that the 4 mg dose significantly improved signs and symptoms of active SLE in patients who were not adequately controlled despite standard-of-care therapy [6]. However, patients included in this trial had low skin activity, and showed no improvement in skin symptoms.
The type I interferon (IFN) system plays a key role in SLE pathogenesis: increased expression of type I IFN-regulated proteins can be found in the blood and target tissues of patients with CLE and SLE [7]. Cell signalling by all type I IFNs is mediated by the IFN-alpha receptor (IFNAR) [8]. This is the rationale for developing IFNAR antibodies. In a phase 2b, randomised, double-blind, placebo-controlled study, the efficacy and safety of the IFNAR antagonist anifrolumab was assessed [9]. Therapy with anifrolumab led to at least 50% improvement in the Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI) in patients with CLASI activity score ≥10 at baseline [9]. In this study, therapy had a greater effect size in patients with a high IFN signature at baseline.
Prof. Werth concluded that “SLE patients will probably benefit most from combination therapy – similar to the situation in oncology.”
- Werth V. 24th World Congress of Dermatology, 10-15 June 2019, Milan, Italy.
- Merrill JT, et al. Lupus Sci Med 2018;5:e000284.
- Van Vollenhoven, RF et al. Lancet 2018;392:1330-39.
- Manzi S, et al. Ann Rheum Dis 2012;71:1833-8.
- Mok CC. Int J Rheum Dis 2015;18:154-63.
- Wallace DJ, et al. Lancet 2018;392:222-31.
- Braunstein I, et al. Br J Dermatol 2012;166:971-5.
- Ivashkiv LB, et al. Nat Rev Immunol 2014;14:36-49.
- Furie R, et al. Arthritis Rheumatol 2017;69:376-386.
Posted on
Previous Article
« Novel selective IL-23 blocker highly effective over 2 years Next Article
Treating keloids with lasers »
« Novel selective IL-23 blocker highly effective over 2 years Next Article
Treating keloids with lasers »
Table of Contents: WCD 2019
Featured articles
Letter from the Editor
Insights into pathogenesis of AD define novel therapeutic targets
Treating Psoriasis in 2019
Choosing the right biologic in psoriasis
Registries – an important research tool in biologics
Atopic Dermatitis – What is New
Insights into pathogenesis of AD define novel therapeutic targets
Combinations are hot in AD treatment
Dermal Reactions to Systemic Drugs
Cutaneous adverse events due to EGFR inhibitors
Management strategies for drug-induced mucositis
Skin toxicity of immune checkpoint inhibitors
Lupus Erythematosus Today
New targets and biologics for cutaneous lupus erythematosus
Novel lupus classification will aid future research
Hidradenitis Suppurativa
Various guidelines with much overlap
Antibiotics in hidradenitis suppurativa
Biologicals beyond TNF blockade
Small Molecules – What to Expect
Novel treatment options for many dermatologic indications
Long awaited oral therapy for moderate-to-severe AD
Novel treatment options in alopecia areata and vitiligo
Optimising the Management of Keloids
Keloids: a faulty switch in wound healing?
What the future of keloid treatment could hold
Malignant Melanoma – Advances in Management
Will malignant melanoma become a curable disease?
Best of the Posters
Related Articles
May 17, 2022
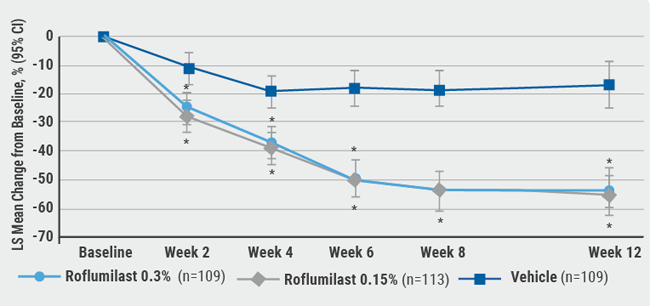
Novel developments in topical psoriasis therapy
August 6, 2020
A new topical PDE-4 inhibitor effective in psoriasis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

