AK is an intraepidermal proliferation of dysplastic keratinocytes that develops in response to chronic exposure to UV radiation. There are numerous treatment methods. One of the most effective is PDT, which involves the use of a topical photosensitising agent such as methyl aminolevulinate (MAL) before exposure to an activating light source to generate reactive oxygen species that lead to cell death. However, stratum corneum is a major barrier for drug permeation, thus decreasing transdermal MAL uptake. Therefore, different pretreatment options have been assessed to enhance PDT efficacy, including microdermabrasion, microneedling, and ablative fractional laser pretreatment. The latter has been shown in a previous study to be effective in enhancing the penetration and accumulation of photosensitisers [2].
In the present study, Dr Yeo-Rye Cho (Dong-A University Busan, Korea) and her colleagues assessed whether there are differences dependent on the chosen laser channel density of the microscopic ablation zones. Korean patients (n=47) with 312 AK lesions were enrolled in the study and treated with 5.5% ablative fractional laser (AFL)-PDT, 11% AFL-PDT, or 22% AFL-PDT and received 1 session of PDT after AFL therapy. Treatment efficacy was determined based on the regression of lesions over time; and accumulated levels of bioconversion to protoporphyrin IX (PpIX), side effects, and cosmetic outcomes were assessed.
Higher channel density associated with higher response rates
No difference was observed in the protoporphyrin IX accumulation between the different groups. "Obviously, the lowest channel density was sufficient to achieve maximum drug penetration," said Dr Cho. However, a significant difference between the complete response rate at 3 months, and in particular at 12 months were noted. After a year, 60.9% of the patient in the 5.5% group compared with 74.0% in the 11% group, and 81.1% in the 22% group showed a complete response (P=0.003). Most benefits were noticed in patients with Olsen grade III lesions, a score for AK that grades severity/thickness of individual AK lesions. After 12 months, 38.2% in the 5.5% group compared with 57.1% in the 11% group and 68.8% in the 22.0% group showed a complete response (P=0.043). “Patients with thick lesions seem to benefit most from the 22% density as the debulking effect is more pronounced,” said Dr Cho. There were no differences with regard to side effects; rates of erythema were similar in all 3 groups. In addition, the cosmetic effect was comparable. There were no differences with regard to side effects; rates of erythema were similar in all three groups. In addition, the cosmetic effect was comparable.
"As AK with severe hyperkeratosis showed a better long-term complete response rate with lesser recurrences, we recommend AFL with higher laser channel density when AFL-PDT is used to treat AK with severe hyperkeratosis," concluded Dr Cho.
1. Cho Y-R. Abstract 11263, AAD Annual Meeting, 1-5 March 2019, Washington DC, USA.
2. Ko DY, et al. J Eur Acad Dermatol Venereol 2014;28:1529-39.
Posted on
Previous Article
« Tralokinumab improves eczema and reduces staphylococcus aureus colonisation in AD Next Article
JAK inhibitors: a pathogenesis-directed therapy for alopecia areata »
« Tralokinumab improves eczema and reduces staphylococcus aureus colonisation in AD Next Article
JAK inhibitors: a pathogenesis-directed therapy for alopecia areata »
Table of Contents: AAD 2019
Featured articles
Letter from the Editor
Interview with AAD president Prof. George J. Hruza
Late-Breakers
Secukinumab maintains improvements in psoriasis through 5 years of treatment
Bermekimab – a future treatment for atopic dermatitis?
JAK1/2 inhibitor effective in alopecia areata
Novel anti-IgE drug enables durable urticaria control
Dual IL-17A and IL-17F blocker leads to unprecedented response rates in psoriasis
Thicker AK lesions benefit from laser pretreatment with high channel density
New standardised cantharidin product against molluscum contagiosum efficacious in two phase 3 trials
Bruton’s tyrosine kinase inhibitor highly effective in pemphigus vulgaris
Serlopitant reduces pruritus associated with psoriasis
Atopic Dermatitis: Many New Therapies in the Pipeline
New and emerging atopic dermatitis therapies
Food triggers eczema – an imperturbable belief of patients
Psoriasis and Biologics: The Beat Goes On
Psoriasis and Biologics: The Beat Goes On
JAK Inhibitors: A New Frontier in Dermatology
JAK inhibitors: a new therapeutic tool for dermatologists
JAK inhibitors: a pathogenesis-directed therapy for alopecia areata
Can JAK inhibitors close the current therapeutic gap in AD?
Hair Loss: No Reason for Therapeutic Nihilism
Hair Loss: No Reason for Therapeutic Nihilism
Vitiligo: The Beginning of a New Era
Vitiligo in children
Surgical treatment for selected vitiligo cases
JAK-inhibitors: an emerging treatment option for vitiligo
What's New and Hot in Acne
Should we use more hormonal therapy?
Pearls of the Posters
Pemphigus patients prone to osteoporosis
Intralesional 5-fluorouracil induced high clearance rates in cutaneous squamous cell carcinoma
Related Articles

November 26, 2019
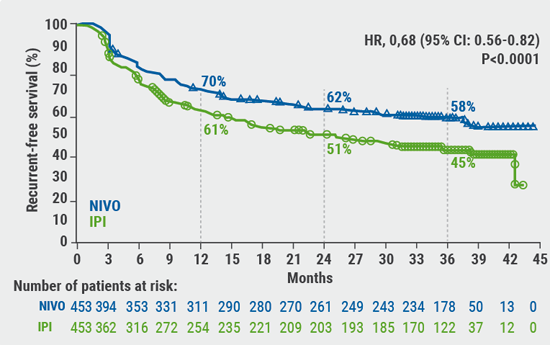
Adjuvant nivolumab provides benefit
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

