The topical tyrosine kinase (TYK)2/Janus kinase (JAK)1 inhibitor brepocitinib is a single-molecule designed to target 2 key pathways that play a role in both psoriasis and AD. Inhibition of TYK2 blocks the Th17 axis, which is important in psoriasis but also in specific forms of AD, for example in Asian patients with AD and paediatric new-onset AD. In contrast, inhibition of JAK1 blocks the Th2-pathway, the relevant pathway in European and American AD patients.
Prof. Megan Landis (University of Louisville School of Medicine, USA) presented promising results of a double-blind, vehicle-controlled, phase 2b study that assessed the efficacy and safety of topical brepocitinib in patients with mild-to-moderate AD. The study randomised 292 adult and adolescent AD patients with mild-to-moderate disease (i.e. Investigators Global Assessment [IGA] 2-3 and a. Eczema Area and Severity Index [EASI] total score of ≥3 to ≤21), who received at least 1 dose of the study drug or vehicle cream. The study period of 6 weeks was completed by 240 patients. The primary endpoint was the percentage change from baseline in EASI total score at week 6. In addition, the EASI 90 response and the proportion of participants achieving an IGA score of clear (0) or almost clear (1) skin and a reduction from baseline of ≥2 points at week 6 were assessed as secondary endpoints.
At week 6, a significant decrease from baseline in EASI score was seen with the cream that contained 1% brepocitinib, which was the highest BID dose tested in the study. When brepocitinib was applied twice daily, there was a 75% decrease in EASI score compared with 47.6% in the vehicle group. A significant treatment response was also seen in the secondary endpoints. Participants treated with the cream containing 0.3%, 1.0%, and 3.0% brepocitinib twice daily achieved significantly more often an EASI 90 response compared with the vehicle group. A significantly higher percentage of patients in all brepocitinib groups achieved an IGA 0/1 response at week 6.
The influence on pruritus, a symptom particularly bothering AD patients, was also assessed as the percentage of participants achieving a ≥4-grade reduction from baseline (among those with baseline ≥4 in severity on the peak pruritus numerical rating scale). “A significant effect on pruritus was observed in the 2 highest doses,” Prof. Landis said. This reduction was achieved by 50% of the participants treated once-daily with the 3.0% brepocitinib cream (see Figure).
“With regard to safety, we noticed no side effects that increased with dose. We also had no serious adverse events and no lab changes,” Prof. Landis reported. Of note, more patients in the vehicle group had side effects or discontinued the study due to treatment-emergent adverse events than in the brepocitinib groups. “This trial supports the use of this novel agent for patients with mild-to-moderate AD,” Prof. Landis concluded.
Figure: Participants achieving ≥4-grade reduction from baseline among those with baseline ≥4 in PP-NRS at week 6 (FAS, NRI) [1]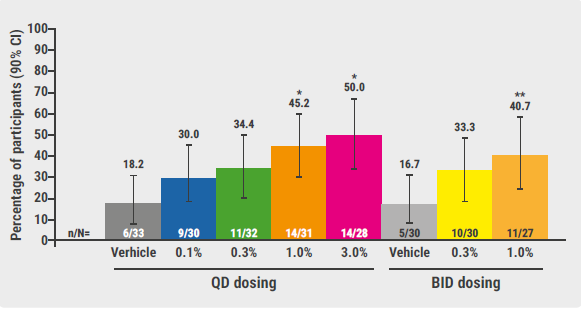 Unadjusted, one-sided P-values: *P≤0.05 versus vehicle once daily; ** P≤0.05 versus vehicle twice daily.
Unadjusted, one-sided P-values: *P≤0.05 versus vehicle once daily; ** P≤0.05 versus vehicle twice daily.
BID, twice daily; CI, confidence interval; FAS, full analysis set; NRI, non-responder imputation; PP-NRS, Peak Pruritus Numerical Rating Scale; QD, once daily.
- Landis M, et al. A Phase 2b study to evaluate the efficacy and safety of the topical TYK2/JAK1 inhibitor brepocitinib for mild-to-moderate atopic dermatitis. Late-breaking abstract D1T03.4D, EADV 2020 Virtual Congress, 29-31 Oct.
Posted on
« Biologic psoriasis treatment and COVID-19 risk: Contradictory results Next Article
JAK1 inhibition successful in hidradenitis suppurativa »
Table of Contents: EADV 2020
Featured articles
Late-Breaking News
Selective IL-23 blocker shows potential in psoriasis treatment
Promising results with nanobody treatment in psoriasis
Light at the end of the tunnel for chronic hand eczema
Epidermolysis bullosa: Novel wound treatment on the horizon
Efficacious non-steroidal topical for psoriasis
Oral JAK 1 inhibitor leads to fast itch relieve and remarkable skin clearance in AD
COVID-19: What Dermatologists Need to Know
Biologic psoriasis treatment and COVID-19 risk: Contradictory results
Much to be learned about COVID-19 and the skin
JAK Inhibitors – A Fascinating Novel Drug Class
JAK inhibitors in AA: re-establishing the immune privilege of hair follicles
JAK1 inhibition successful in hidradenitis suppurativa
Topical JAK inhibition: a novel treatment option for patients with mild-to-moderate AD
Urticaria – What’s new
Chronic inducible urticaria can require some detective work
Chronic spontaneous urticaria: hives, wheals & biomarkers
Ligelizumab for chronic spontaneous urticaria: a new star on the horizon
Infectious Diseases: Novel Developments
Bacterial resistance in skin infections – a challenging threat
Borreliosis: A multifaceted disease
Scabies – A global health challenge
Upcoming Treatments
Meaningful sleep improvement with IL-13 inhibition
Preventing foot odour with zinc oxide coated socks
Baricitinib in AD: Efficacy paired with consistent long-term results
Best of the Posters
Real-world data on brodalumab affirms efficacy and fast onset of action
Heightened risk for psychiatric comorbidities in hidradenitis suppurativa patients
Effects IL-13 blocker improves with longer treatment duration
Related Articles

EADV 2020 Highlights Podcast
Scabies – A global health challenge
Bacterial resistance in skin infections – a challenging threat
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

