Tralokinumab is an anti-IL-13 monoclonal antibody that has previously demonstrated significant superior efficacy in reducing signs and symptoms of atopic dermatitis (AD) in the pivotal phase 3 trials ECZTRA 1 (NCT03131648) and ECZTRA 2 (NCT03160885) [1]. As sleep loss plays a major role in the decreased quality of life of AD patients, Prof. Jonathan Silverberg (George Washington University School of Medicine and Health Sciences, USA) and his fellow researchers performed a post-hoc analysis of these studies with a focus on the impact of tralokinumab on sleep loss [2,3]. The identically designed, international studies randomised over 1,500 adult patients to receive either tralokinumab 300 mg every 2 weeks over 16 weeks or placebo [3]. In ECZTRA trials, 3 different kinds of sleep measures were evaluated: the eczema-related sleep Numeric Rating Scale (NRS) with a 24-hour recall, the Scoring Atopic Dermatitis (SCORAD) sleep score with a 3-day recall, and the Patient Oriented Eczema Measure (POEM) sleep score with a 7-day recall. The NRS data was collected in an e-diary filled out by the patients themselves, data for SCORAD and POEM was gathered during the study visits.
“Baseline characteristics were similar between the groups, really everything was well balanced across trials and across treatment arms,” said Prof. Silverberg. For example, in ECZTRA 1, the mean Eczema Area and Severity Index (EASI) was 32.9 in the placebo arm versus 32.2 in the tralokinumab arm. The respective measures for sleep were: 6.8 versus 6.9 for the sleep NRS, 6.4 versus 6.5 for the sleep SCORAD, respectively, and 3.3 for POEM. The mean age of the participants was 39, about 60% of patients were male.
The results for eczema-related sleep disturbance in the NRS showed greater improvements in both tralokinumab arms. “The curves for tralokinumab show early separations already by week 1 compared with placebo, and that separation continues to widen even further and continues out to week 16 and it is really statistically significant at all endpoints,” Prof. Silverberg highlighted. The P-values at every week versus placebo were all either P<0.01 or P<0.001. At week 16, changes from baseline were -2.6 for tralokinumab versus -1.9 for placebo in ECZTRA 1, and -2.9 for tralokinumab versus -1.5 for placebo in ECZTRA 2. Results in SCORAD sleep score were similar: at week 16, the difference was -2.6 and -3.0 for tralokinumab versus -1.8 and -1.8 for placebo with a P<0.01 and P<0.001 in ECZTRA 1 and ECZTRA 2, respectively.
POEM is a categorical scale placing the days of sleep disturbance in 5 different classes starting at 0 days, then 1-2 days, and further up to every day. “At baseline almost everybody had really profound sleep disturb with ≥3 nights of disturbed sleep,” said Prof. Silverberg. At week 16, there were higher proportions of patients who even achieved 0, or only 1 or 2 night of sleep problems in the tralokinumab groups, without much amelioration in the placebo arms. For example, in ECZTRA 2, at baseline, 14% of patients reported up to 6 days and 65.4% everyday sleep disturbance within the tralokinumab arm. The corresponding proportion in the placebo arm were 11% and 68%, respectively. At week 16, the percentage of tralokinumab recipients with everyday sleep problems declined to 33.3%, and 39.1% even reported 0 or only 1-2 disturbed nights, while the matching placebo rates were 51.5% and 21.5%.
“Early improvement in sleep measures as early as week 1 with tralokinumab is consistent with its effects on the signs and troublesome symptoms of atopic dermatitis, including pruritus,” concluded Prof. Silverberg.
- Wollenberg A, et al. Br J Dermatol. 2020 Sep 30. DOI:10.1111/bjd.19574.
- Chang YS, et al. J Allergy Clin Immunol. 2018;142:1033-40.
- Silverberg J, et al. Specifically targeting interleukin-13 with tralokinumab improved sleep in two Phase 3, randomised, double-blind, placebo-controlled trials in patients with atopic dermatitis. FC08.05, EADV 2020 Virtual Congress, 29-31 Oct.
Posted on
Previous Article
« Preventing foot odour with zinc oxide coated socks Next Article
Heightened risk for psychiatric comorbidities in hidradenitis suppurativa patients »
« Preventing foot odour with zinc oxide coated socks Next Article
Heightened risk for psychiatric comorbidities in hidradenitis suppurativa patients »
Table of Contents: EADV 2020
Featured articles
Late-Breaking News
Selective IL-23 blocker shows potential in psoriasis treatment
Promising results with nanobody treatment in psoriasis
Light at the end of the tunnel for chronic hand eczema
Epidermolysis bullosa: Novel wound treatment on the horizon
Efficacious non-steroidal topical for psoriasis
Oral JAK 1 inhibitor leads to fast itch relieve and remarkable skin clearance in AD
COVID-19: What Dermatologists Need to Know
Biologic psoriasis treatment and COVID-19 risk: Contradictory results
Much to be learned about COVID-19 and the skin
JAK Inhibitors – A Fascinating Novel Drug Class
JAK inhibitors in AA: re-establishing the immune privilege of hair follicles
JAK1 inhibition successful in hidradenitis suppurativa
Topical JAK inhibition: a novel treatment option for patients with mild-to-moderate AD
Urticaria – What’s new
Chronic inducible urticaria can require some detective work
Chronic spontaneous urticaria: hives, wheals & biomarkers
Ligelizumab for chronic spontaneous urticaria: a new star on the horizon
Infectious Diseases: Novel Developments
Bacterial resistance in skin infections – a challenging threat
Borreliosis: A multifaceted disease
Scabies – A global health challenge
Upcoming Treatments
Meaningful sleep improvement with IL-13 inhibition
Preventing foot odour with zinc oxide coated socks
Baricitinib in AD: Efficacy paired with consistent long-term results
Best of the Posters
Real-world data on brodalumab affirms efficacy and fast onset of action
Heightened risk for psychiatric comorbidities in hidradenitis suppurativa patients
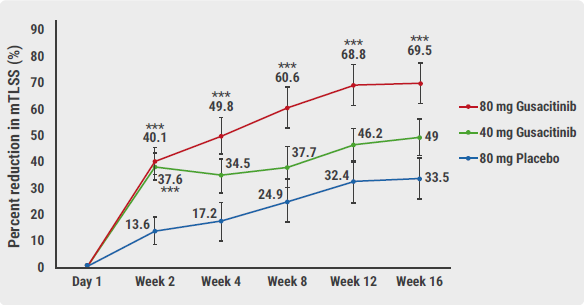
Effects IL-13 blocker improves with longer treatment duration
Related Articles
December 17, 2020
Light at the end of the tunnel for chronic hand eczema
December 17, 2020
Borreliosis: A multifaceted disease
December 17, 2020
Preventing foot odour with zinc oxide coated socks
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

