https://doi.org/10.55788/93769d25
As the diagnosis of psoriasis has been linked to an increased risk of MACE and thromboembolic events, knowledge about a potential further increase of risk through anti-inflammatory medication is important [1,2]. In this context, Prof. Mark Lebwohl (Icahn School of Medicine at Mount Sinai, NY, USA) and colleagues investigated exposure-adjusted incidence rates of MACE and VTE in the treatment of psoriasis with the TYK2 inhibitor deucravacitinib [1]. The analysis was performed on data from the phase 3 POETYK PSO-1 and PSO-2 studies (NCT03624127 and NCT03611751), evaluating deucravacitinib against placebo and apremilast. After week 16, >95% of the participants in both trials continued on deucravacitinib until week 52 in a long-term extension study (NCT04036435). MACE were defined as non-fatal myocardial infarction or stroke, as well as CV death, and VTE comprised pulmonary embolism and deep vein thrombosis. Pooled data of all 3 trials with analysis cut-off in June 2021 included 2,166.9 deucravacitinib person-years (PY) and a median exposure time of 588 days.
The baseline characteristics of PSO-1 and PSO-2 demonstrated 31.3% hypertensive, 11.3% obese, 10.4% hyperlipidemic, and 10.3% diabetic participants. Adverse events up to week 16 were mostly mild to moderate and comparable among the study arms. However, adverse events involving drug discontinuation varied: the exposure-adjusted incidence rates were 17.9/100 PY for apremilast, 13.2/100 PY for placebo, and 8.0/100 PY for deucravacitinib. The corresponding exposure-adjusted incidence rates for weeks 0–52 were 11.6/100 PY, 9.3/100 PY, and 4.4/100 PY, for apremilast, placebo, and deucravacitinib, respectively. Nasopharyngitis and upper respiratory infection were the most common adverse events on deucravacitinib, while headache and diarrhoea were the most frequent on apremilast. MACE by adjudication through an external CV committee also varied according to therapy. In the 1-year safety pool, the placebo arm’s incidence amounted to 1.2 exposure-adjusted incidence rates/100 PY, compared with 0.9 exposure-adjusted incidence rates/100 PY with apremilast and 0.3 exposure-adjusted incidence rates/100 PY on deucravacitinib. In terms of VTE from weeks 0–52, the rate among deucravacitinib-treated participants was 0.1 exposure-adjusted incidence rates/100 PY.
The investigators concluded that despite the high proportion of participants with baseline CV risk factors, MACE and VTE were low overall and did not increase with a longer duration of deucravacitinib treatment. Thus, in their opinion, deucravacitinib treatment has a favourable safety profile.
- Lebwohl M, et al. Deucravacitinib, an oral, selective tyrosine kinase 2 (TYK2) inhibitor: major adverse cardiovascular events (MACE) and venous thromboembolic events (VTEs) in the phase 3 POETYK PSO-1, PSO‑2, and long-term extension (LTE) trials. P078, SPIN 2022 Congress, 06–08 July, Paris, France.
- Chen TL, et al. JAMA Dermatol. 2022;158:59-67.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Comorbid anxiety and depression may benefit from psoriasis treatment with certolizumab Next Article
Alopecia areata pathogenesis: known genetic background, unknown environmental triggers »
« Comorbid anxiety and depression may benefit from psoriasis treatment with certolizumab Next Article
Alopecia areata pathogenesis: known genetic background, unknown environmental triggers »
Table of Contents: SPIN 2022
Featured articles
Letter from the Editor
IMIDs in Adults and Children: New Developments
Therapies for atopic dermatitis: still moving forward
Children with AD: high risk of bacterial infections in carriers of a filaggrin gene variant
Men on biologics report fewer adverse events than women
Conceptual framework of adverse drug reactions may improve treatment of patients with IMIDs
Psoriasis: The Beat Goes On
Systemic treatment for psoriasis: what is on the horizon?
Topical therapy in psoriasis: an important partner in combination therapy
GPP flares: pronounced undertreatment is common
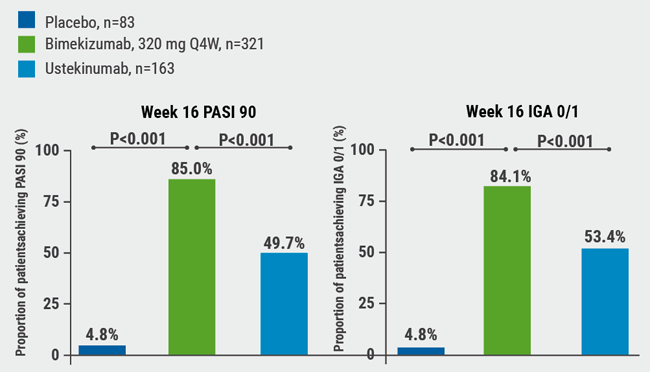
IL-17A/F inhibitor bimekizumab shows higher response and maintenance rates compared with secukinumab
Paediatric psoriasis: ixekizumab beneficial in difficult-to-treat areas
Psoriasis patients see great benefit in achieving complete skin clearance
The Future Is Bright for Vitiligo
Predilection sites for skin signs of vitiligo disease activity determined
Where Are We Now in Hidradenitis Suppurativa
IHS4 better suited as an outcome measure in HS trials?
New treatments for HS: IL-17 inhibitors next in practice?
New Treatment Options in Alopecia Areata
Alopecia areata: light at the end of the tunnel
Alopecia areata pathogenesis: known genetic background, unknown environmental triggers
Best of the Posters
Psoriasis treatment: no elevation of MACE and VTE on deucravacitinib
Comorbid anxiety and depression may benefit from psoriasis treatment with certolizumab
Dose tapering in psoriasis is associated with a low relapse rate
Related Articles
August 26, 2022
GPP flares: pronounced undertreatment is common
August 6, 2020
IL-17A and IL-17F blockade remarkably effective in psoriasis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

