The oral JAK1/JAK2 inhibitor baricitinib has shown significant efficacy in improving signs and symptoms of AD in the 2 independent monotherapy trials BREEZE-AD1 (NCT03334396) and BREEZE-AD2 (NCT03334422) [1]. Patients completing these studies were eligible for enrolment into the presented BREEZE-AD3 (NCT03334435), a double-blind, long-term extension trial to assess baricitinib in patients with moderate-to-severe AD up to 68 weeks [2].
The trial design differed depending on the participant’s outcome at the end of the parent studies. Responders and partial responders, identified by a validated Investigator´s Global Assessment (IGA) for AD of 0, 1, or 2 at week 16, would continue receiving the same agent as in BREEZE-AD1 and BREEZE-AD2. As a result, there were 4 arms with either placebo or 1 mg, 2 mg, or 4 mg of baricitinib. Non-responders, who ended the previous studies with an validated IGA AD score of 3 or 4, were re-randomised and switched from once daily placebo, 1 mg, or 2 mg of baricitinib to either 2 mg or 4 mg of baricitinib in the extension study. Non-responders in the 4 mg baricitinib group continued their previous dosage. Efficacy outcomes were measured by the rate of patients achieving a validated IGA AD of 0/1 (i.e. clear or almost clear) as the primary endpoint and an Eczema Area and Severity Index (EASI) 75 improvement up to 68 weeks. The investigators used 2 different approaches for imputing missing data: last observation carried forward (LOCF) and non-responder imputation (NRI). Results were compared between both methods.
Independent of the applied approach, baricitinib 4 mg accounted for an overall consistent efficacy that was more or less maintained from week 16 on, with a validated IGA AD 0/1 starting at 45.7% at week 16 and reaching 47.1% (LOCF) and 40.0% (NRI) at week 68. Furthermore, the EASI 75 of 70.0% at week 16 decreased slightly to 55.7% (LOCF) and 51.4% (NRI) at week 68 (see Figure). Similar outcomes were seen in the evaluation of itch NRS (≥4-point improvement), skin pain NRS (≥4-point improvement), and AD symptom score (ADSS) item 2 (≥1.5-point improvement) with baricitinib 4 mg. “You see a consistent pattern across all those endpoints regardless of using LOCF or NRI,” said Prof. Jonathan Silverberg (George Washington University School of Medicine and Health Sciences, USA). The rates measured at week 32 (LOCF) were: 45.9% (itch NRS), 54.5% (skin pain NRS), and 71.4% (ADSS item 2) versus 52.5%, 61.8%, and 75.0%, respectively, at week 16. In the baricitinib 2 mg treatment arms, validated IGA AD and EASI 75 percentages at week 16 were 46.3% and 74.1%, and even mounted to 59.3% and 81.5% (both with LOCF) at week 68. Also, the patient-related outcomes were suggestive of stable response through week 32.
Figure: Results for validated IGA AD 0/1 and EASI 75 with baricitinib 4 mg from week 16 to 68 [2]

*Total weeks includes the 16 weeks of treatment in the original studies BREEZE-AD1 and BREEZE-AD2.
EASI, Eczema Area and Severity Index; LOCF, last observation carried forward; NRI, non-responder imputation; vIGA-AD, validated Investigator’s Global Assessment for atopic dermatitis.
Reassuring safety data in over 2,500 treated patients
Since the patients enrolled in BREEZE-AD3 originated from different parent studies, Prof. Silverberg presented a unique safety summary that was published, which contained integrated data from 2,531 patients from 8 clinical trials (7 phase 3 trials and a phase 2 trial) [2,3]. The data includes adverse event information from responders, partial responders, and non-responders within the placebo-controlled data sets until week 16, as well as the extended analyses. All AD trial patients treated with baricitinib equalled a total of 2247.4 patient-years of exposure. “What you can appreciate overall is that the safety is pretty consistent to what we have seen in the individual studies, but now in the pooled analyses there is maybe a little bit of an increase in terms of any treatment-related adverse events with baricitinib 2 mg and 4 mg doses, although we don’t see any kind of dose-dependent responses,” Prof. Silverberg pointed out. Especially in the placebo-controlled treatment phase up to week 16, there were no deaths, no gastro-intestinal perforations, and no major adverse cardiovascular events. In all patients treated with baricitinib (n=2,531), herpes zoster had a study size-adjusted incidence rate of 2.3 and herpes simplex an incidence rate of 10.3. All in all, authors of the safety analysis observed no new safety concerns. In conclusion, Prof. Silverberg highlighted that baricitinib 2 mg and 4 mg demonstrated sustained long-term efficacy in moderate-to-severe AD.
- Simpson EL, et al. Br J Dermatol. 2020;183:242-55.
- Silverberg JI, et al. Long-term efficacy of baricitinib in patients with moderate-to-severe atopic dermatitis enrolled in the phase 3 long-term extension study BREEZE-AD3. D3T03.4a, EADV 2020 Virtual Congress, 29-31 Oct.
- Bieber T, et al. J Eur Acad Dermatol Venereol. 2020 Sep 14. Doi: 10.1111/jdv.16948.
Posted on
Previous Article
« Bacterial resistance in skin infections – a challenging threat Next Article
Preventing foot odour with zinc oxide coated socks »
« Bacterial resistance in skin infections – a challenging threat Next Article
Preventing foot odour with zinc oxide coated socks »
Table of Contents: EADV 2020
Featured articles
Late-Breaking News
Selective IL-23 blocker shows potential in psoriasis treatment
Promising results with nanobody treatment in psoriasis
Light at the end of the tunnel for chronic hand eczema
Epidermolysis bullosa: Novel wound treatment on the horizon
Efficacious non-steroidal topical for psoriasis
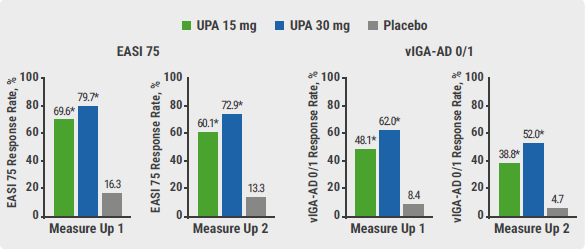
Oral JAK 1 inhibitor leads to fast itch relieve and remarkable skin clearance in AD
COVID-19: What Dermatologists Need to Know
Biologic psoriasis treatment and COVID-19 risk: Contradictory results
Much to be learned about COVID-19 and the skin
JAK Inhibitors – A Fascinating Novel Drug Class
JAK inhibitors in AA: re-establishing the immune privilege of hair follicles
JAK1 inhibition successful in hidradenitis suppurativa
Topical JAK inhibition: a novel treatment option for patients with mild-to-moderate AD
Urticaria – What’s new
Chronic inducible urticaria can require some detective work
Chronic spontaneous urticaria: hives, wheals & biomarkers
Ligelizumab for chronic spontaneous urticaria: a new star on the horizon
Infectious Diseases: Novel Developments
Bacterial resistance in skin infections – a challenging threat
Borreliosis: A multifaceted disease
Scabies – A global health challenge
Upcoming Treatments
Meaningful sleep improvement with IL-13 inhibition
Preventing foot odour with zinc oxide coated socks
Baricitinib in AD: Efficacy paired with consistent long-term results
Best of the Posters
Real-world data on brodalumab affirms efficacy and fast onset of action
Heightened risk for psychiatric comorbidities in hidradenitis suppurativa patients
Effects IL-13 blocker improves with longer treatment duration
Related Articles
December 17, 2020
Borreliosis: A multifaceted disease
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

