When assessing patients for surgery, one of the key elements is patient counselling to adjust expectations and inform the patient (and caregiver) on various subjects. These include expected course, surgery logistics, practical issues (e.g., preventing dehydration in patients who will have a stoma fitted), and stoma pre-operative counselling. Giving information decreases post-operative anxiety [1].
Surgery has undergone a revolution in recent years: enhanced recovery pathways have been developed and minimally invasive surgery has become the gold standard in IBD. The goals of minimally invasive surgery go beyond the single fact of leaving behind smaller scars. Minimising surgical trauma has many benefits such as shorter hospital stay, less (work-related and social) inactivity, less disability, decreased fears and anxiety of patients, etc.
A study by Spinelli et al. combined laparoscopy with an enhanced recovery pathway in 20 patients with CD [2]. This included no bowel preparation nor fasting, no nasogastric tube, no abdominal drains, and early removal of the urinary catheter. In addition, early solid dietary intake and mobilisation, opioid-sparing analgesia, and restrictive fluid management were instituted. The results showed that compliance with the enhanced recovery pathway was high (≥80%) for all items except no drain placement. Also, a significantly earlier return of bowel function (time to first flatus and stool) was observed in the patients who had been subject to the enhanced recovery pathway.
The historical control group consisted of 70 CD patients who underwent laparoscopic ileocecal resection and were treated with conventional care. Mean post-operative and total length of stay were significantly shorter in the enhanced recovery pathway group. Post-operative complications were similar in both patient groups. A multimodal pain management strategy is recommended, where two or more analgesics which act on different mechanisms at different sites are used simultaneously. A step strategy to minimise opioids and related AEs also leads to adequate pain control, earlier return of bowel function, and shorter hospitalisation [3].
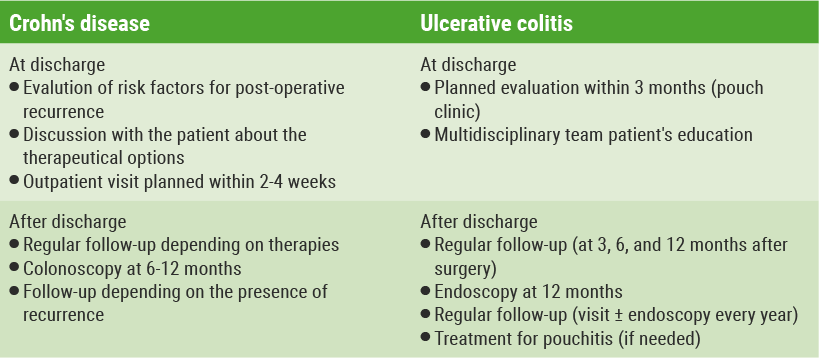
Additional perioperative measures include preventing nausea and vomiting, surgical site infection, and thromboembolic events (low molecular weight heparin and mobilisation). Over-infusion should also be avoided, as there is a linear relation to complication [4-10]. After the patient has been discharged from hospital, follow-up is essential; this should be done at specific time-points, depending on the condition (see Table) [11].
Table: Timing follow-up post-surgery [11]
- Millan M, et al. Colorectal Dis. 2010;12(7 Online):e88-92.
- Spinelli A, et al. J Gastrointest Surg. 2013;17(1):126-32.
- Larson DW, et al. Br J Surg. 2014;101(8):1023-30.
- Franck M, et al. J Int Med Res. 2010;38(3):1034-41.
- Eberhart LH, et al. Anaesthesia. 2002;57(10):1022-7.
- Tanner et al. Surgery. 2015;158:66-77.
- Gorgun E, et al. Dis Colon Rectum. 2018;61(1):89-98.
- Colorectal Writing Group for Surgical Care and Outcomes Assessment Program–Comparative Effectiveness Research Translation Network (SCOAP-CERTAIN) Collaborative. JAMA Surg. 2015;150(8):712-20.
- Brandstrup B, et al. Ann Surg. 2003;238(5):641-8.
- Regenbogen SE, et al. Ann Surg. 2017;265:930-940.
- Fiorino G. ECCO 2018.
Posted on
Previous Article
« Combining new drugs with different mechanisms Next Article
Quiescent disease, characteristics and biomarker correlations »
« Combining new drugs with different mechanisms Next Article
Quiescent disease, characteristics and biomarker correlations »
Table of Contents: ECCO 2018
Featured articles
IBD diagnostics
IBD disease patterns and genetics
Novel treatment strategies
Efficacy and safety of biologics
Oncology in IBD
Surgery for IBD
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com


