The suggested correlation between appendectomy and UC was investigated in a meta-analysis; at the same time, possible confounding factors were analysed.
A systematic review and meta-analysis were performed in July 2017 using MEDLINE, EMBASE and the Cochrane library. Data from studies describing the influence of appendectomy on colectomy rate and risk of CRC and/or HGD were extracted from published reports. Exclusion criteria were patients <18 years, non-UC, and animal studies.
A total of 891 studies were collected, of which 13 studies evaluating 73,323 UC patients were included (appendectomy n=2,859). All studies except one were rated as poor quality. Overall, colectomy rate in appendectomised and non-appendectomised patients was not significantly different (OR 1.21, 95% CI 0.84-1.75).
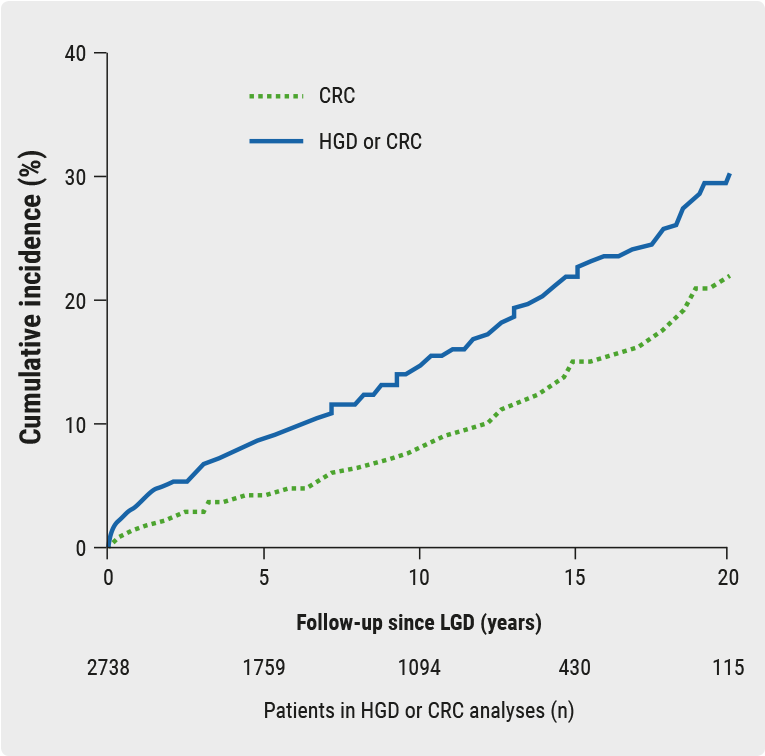
Four of six studies demonstrated significantly longer disease duration, however, with a decreased use of steroids after appendectomy. A total of six studies investigated the risk of CRC and/or HGD, which was significantly increased after appendectomy (OR 3.68, 95% CI 1.70-7.94).
Three studies looked at CRC specifically, which showed the same trend although not significantly so (OR 5.50, 95% CI 0.95-31.96). The increased incidence of malignant degeneration seemed related to longer disease duration. Average disease duration was 102.7 months in the appendectomy group vs. 76.6 months in the non-appendectomy group. Also, the cumulative percentage of primary sclerosing cholangitis was higher in appendectomised patients (13.7%) than in non-appendectomised patients (4.4%). Thus, a significantly increased risk of CRC and/or HGD after appendectomy in UC patients was found, which is presumably correlated with delayed colectomy.
This finding shows that there is no need to stop on-going trials, but emphasises the importance of endoscopic surveillance in high-risk patient groups [8].
- Stellingwerf ME, et al. DOP083. ECCO 2018.
Posted on
Previous Article
« Integration of “omics” and potential for clinical practice Next Article
SHP647 is efficacious and well-tolerated in CD »
« Integration of “omics” and potential for clinical practice Next Article
SHP647 is efficacious and well-tolerated in CD »
Table of Contents: ECCO 2018
Featured articles
IBD diagnostics
IBD disease patterns and genetics
Novel treatment strategies
Efficacy and safety of biologics
Oncology in IBD
Surgery for IBD
Related Articles
May 28, 2018
Genetic predisposition for gut barrier dysfunction
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

