Tofacitinib is an oral, small-molecule JAK inhibitor. It has been shown to be safe and effective for the treatment of moderate-to-severe UC in the OCTAVE induction (P2/P3) and maintenance phase (P3) [4]. Long-term safety and efficacy of tofacitinib for UC are currently being evaluated in an on-going, open-label, long-term extension study [5].
Sandborn et al. described an updated integrated analysis of the safety profile of tofacitinib in the UC global clinical development programme. Patients were exposed to tofacitinib for up to 4.4 years [6]. Patients who received placebo or tofacitinib 5 or 10 mg BID were analysed as three cohorts. To begin, an induction cohort (P2/P3 induction, n=1,220); the second was a maintenance cohort (P3 maintenance, n=592). Thirdly, an overall cohort (patients receiving tofacitinib 5 or 10 mg BID in P2, P3, or the open-label extension study, n=1,157).
In total, 1,613 patient-years of exposure were included. Demographics and disease characteristics were generally similar among the treatment groups in each cohort. Proportions and incidence rates were evaluated for AEs of special interest. Opportunistic infections, malignancies, major adverse cardiovascular events, and gastrointestinal perforations were reviewed by independent adjudication committees. In induction studies, AEs of special interest were similar for tofacitinib and placebo groups. In the maintenance cohort, the incidence rate of herpes zoster (HZ) was numerically higher with tofacitinib 5 mg BID (2.1) vs. placebo (1.0). It was significantly higher with tofacitinib 10 mg BID (6.6). Incidence rates for other AEs of interest were similar across treatment groups. For the overall cohort, 84% of patients received an average dose of tofacitinib 10 mg BID. AEs of special interest were death (0.2), serious infection (2.0), opportunistic infections (1.3) and HZ (4.1).
Malignancies – with the exception of non-melanoma skin cancer (NMSC) – were 0.5, NMSC 0.7, major adverse cardiovascular events 0.2, and gastrointestinal perforations 0.2. Tofacitinib treatment in patients with UC was associated with a dose-dependent risk of HZ. Nevertheless, the researchers stated that these results show an overall manageable safety profile of tofacitinib 5 and 10 mg BID in the UC programme. This profile is generally similar to what has previously been reported in the tofacitinib RA programme. With the exception of an increased HZ risk, it is also similar in other UC therapies, including biologics.
- Sandborn WJ, et al. N Engl J Med, 2017:376;1723-36.
- Lichtenstein GR, et al. Am J Gastroenterol. 2017;112(S1). [Abstract 714]
- Sandborn WJ, et al. DOP023. ECCO 2018.
Posted on
Previous Article
« Central role of IL-23 in molecular resistance to anti-TNF therapy Next Article
Shallow whole-genome sequencing predicts future cancer risk of LGD in UC »
« Central role of IL-23 in molecular resistance to anti-TNF therapy Next Article
Shallow whole-genome sequencing predicts future cancer risk of LGD in UC »
Table of Contents: ECCO 2018
Featured articles
IBD diagnostics
IBD disease patterns and genetics
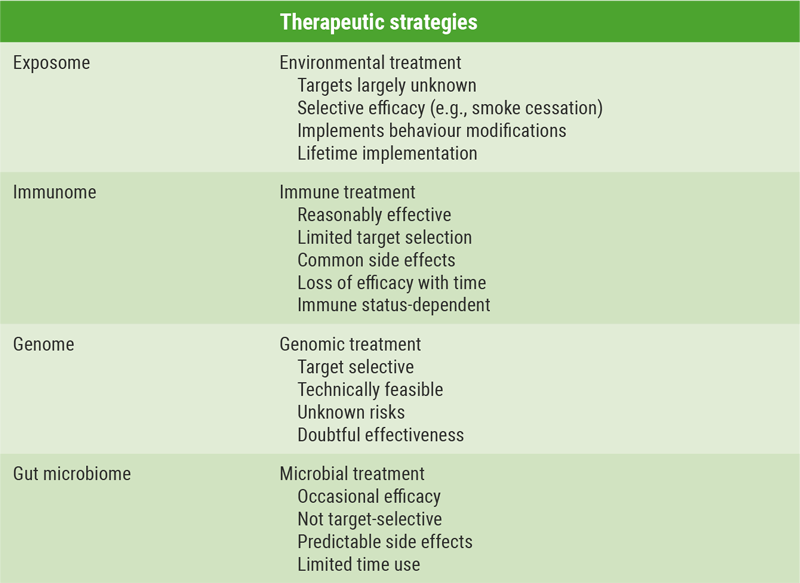
Novel treatment strategies
Efficacy and safety of biologics
Oncology in IBD
Surgery for IBD
Related Articles
May 28, 2018
ILC1 distribution predicts response to ustekinumab
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

