Prof. Scheltens explained that SNAP is a biomarker-based concept denoting AD-like neurodegeneration in individuals without β-amyloidosis. Its prevalence is 20-30% in cognitive healthy individuals; it accounts for 20-40% of patients presenting to memory clinics. SNAP may be caused by cerebrovascular disorders, mixed pathologies (dementia with Lewy bodies, frontotemporal lobar degeneration), or non-AD neurodegeneration, such as primary age-related tauopathy (PART) and limbic-predominant age-related TDP-43 encephalopathy (LATE).
In the ATN system of the National Institute on Ageing-Alzheimer's Association (NIA-AA), 8 major AD biomarkers are divided into 3 pathophysiology-based binary categories. “A” refers to the value of a β-amyloid biomarker (amyloid-PET or cerebrospinal fluid [CSF] Aβ1-42); “T,” the value of a tau biomarker (CSF phosphorylated tau, or tau-PET); and “N,” biomarkers of neurodegeneration or neuronal injury ([18F]-fluorodeoxyglucose-PET, structural MRI, CSF total tau, or neurofilament light chain).
AD risk in individuals with SNAP or with A-T-N- is almost equal. In individuals with mild cognitive impairment (MCI), however, SNAP predicts progression to AD, with a highly variable percentage. In a Dutch study, 3-year progression from SNAP with MCI to AD was 24%, 4 times higher than cognitive healthy individuals [2].
Prof. Scheltens argued that the concept of SNAP is still useful, but that it is now referred to as “non-AD pathophysiology”. This concept is part of a research framework (see Table) proposed by the NIA-AA to define AD pathologies based on ATN profiles [3].
Table. ATN-profiles and corresponding biomarker categories [3].
![Table. ATN-profiles and corresponding biomarker categories [3].](https://conferences.medicom-publishers.com/wp-content/uploads/2020/09/Table.-ATN-profiles-and-corresponding-300x171.png)
1. Scheltens F. Symposium SYMP08, EAN 2020.
2. Vos SJB, et al. Brain. 2015;138(Pt 5):1327-38.
3. Jack Jr CR, et al. Alzheimers Dement. 2018;14(4):535-62.
Posted on
Previous Article
« Novel genetic association with resistance to ERC tau deposition Next Article
Infusion of ethanol in the vein of Marshall for persistent AF »
« Novel genetic association with resistance to ERC tau deposition Next Article
Infusion of ethanol in the vein of Marshall for persistent AF »
Table of Contents: EAN 2020
Featured articles
Alzheimer's Disease and Other Dementias
Non-Alzheimer’s disease pathophysiology in the elderly
Novel genetic association with resistance to ERC tau deposition
Diastolic dysfunction novel risk factor for cognitive impairment
Epilepsy
Avoidable epilepsy-related mortality remains high
How genetic testing can contribute to epilepsy management
Cenobamate effective in focal epilepsy
Sustained seizure reductions with cannabidiol for Lennox-Gastaut syndrome
Prevalence of autoantibodies in epilepsy almost 10%
Parkinson's Disease
White matter matters in Parkinson’s disease
Sleep disorders mark PD progression
Directional DBS superior to omnidirectional DBS
Stroke
Benefits of statins to prevent stroke outweigh risks
Extubation after thrombectomy: the sooner, the better
Thrombus location and length predictors of early neurological deterioration
Endovascular treatment in large vessel occlusion stroke patients treated with OAC
Early edoxaban may be safe after cardioembolic stroke
Headache and Pain
Small fibre pathology as biomarker for fibromyalgia
Migraine as a cyclical functional disorder
Reassuring real-world safety profile of 3 CGRP inhibitors
Long-term cardiovascular safety of erenumab
Real-world data for erenumab in Germany
Eptinezumab in chronic migraine and medication-overuse headache
Fremanezumab tolerability in cardiovascular patients with migraine
Effects of galcanezumab on health-related quality of life
Multiple Sclerosis
Imaging to evaluate remyelination and neuroprotection
Serum NfL predicts long-term clinical outcomes in MS
Epstein-Barr virus-targeted T-cell immunotherapy for progressive MS
High NEDA rates after 2 years of ocrelizumab
Switching from natalizumab to moderate- versus high-efficacy DMT
Results of compounds in late stages of development
Alemtuzumab efficacy and safety data of over 9 years
Fampridine treatment results in routine clinical practice
Air pollution is a possible risk factor for MS
Neuromyelitis Optica Spectrum Disorder
Genetic association studies in NMOSD needed
Eculizumab in NMOSD: the PREVENT study
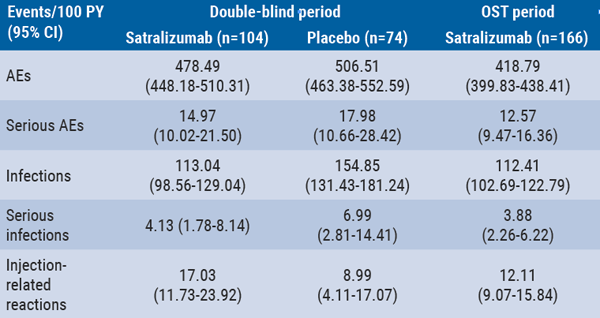
Long-term safety of satralizumab consistent with double-blind periods
Neuromuscular Disorders
Biomarkers predicting motor function in SMA
Sustained benefits of avalglucosidase alfa in late-onset Pompe disease
Efficacy and safety of rituximab in refractory MG corroborated
Related Articles
September 10, 2020
Serum NfL predicts long-term clinical outcomes in MS
September 10, 2020
Long-term safety of satralizumab consistent with double-blind periods
September 9, 2020
Sleep disorders mark PD progression
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

