Presented by Dr Miguel Valderrabano (Baylor College of Medicine, USA), the VENUS trial addressed the challenge of treating persistent AF, which is limited by the imperfect success of catheter ablation procedures, and the consequent need for repeat procedures [1]. The investigators hypothesised that by ablating AF triggers in the VOM through retrograde ethanol infusion, coupled with a catheter ablation approach, the restoration of normal rhythm could be achieved in more patients with persistent AF.
Participants (n=343) with symptomatic persistent AF and refractory to at least 1 anti-arrhythmic agent were randomised to receive either catheter ablation alone (n=158) or catheter ablation combined with VOM ethanol (n=185). The investigators anticipated that approximately 15% of the patients randomised to the VOM group would have a VOM difficult to cannulate; those patients would continue in the study receiving only catheter ablation.
Outcomes were measured at 1, 3, 6, 9, and 12 months post-procedure, with continuous month-long monitoring taking place at the 6- and 12-month time points. Prior to catheter ablation, patients in the VOM group received a coronary sinus venogram to identify the VOM and angioplasty balloon cannulation with 4 retrograde injections of 1 cc of ethanol (from distal to proximal). Left atrial voltage maps were performed before and after the ethanol injection to assess the scar induced by the alcohol administration. Catheter ablation for both groups included pulmonary vein isolation. The extent of the total tissue ablated was determined by a final left atrial voltage map. The primary endpoint at 3 months was resolution of either AF or atrial tachycardia (AT) for more than ≥30 seconds, without anti-arrhythmic medication.
A total of 142 participants were included in the per-treatment analysis; the VOM procedure was unsuccessful in 30 patients, 3 patients died, and 10 participants had missing data. Notably, more patients in the VOM group had hypertension (77% vs 66%) and the atrial diameter was larger in the catheter ablation-only group (44.8 mm vs 47 mm). These distinctions should be considered in the results interpretation.
Resolution of AF or AT for more than 30 seconds after 3 months was achieved in 38% of the patients randomised to the catheter ablation group, and 51.6% among those in the VOM plus catheter ablation group (P=0.015, see Table). AF/AT recurrence was seen in 51.9% of the catheter ablation group, compared with 40% of those undergoing VOM infusion plus catheter ablation.
Table: Ablation success: Resolution of AF or AT ≥30 seconds after 3 months

AF, atrial fibrillation; AT, atrial tachycardia; CI, confidence interval; VOM, vein of Marshall.
Dr Valderrabano concluded: “In persistent AF, VOM ethanol added to catheter ablation reduces the recurrence of AF and AT, reduces the AF, and may reduce the need for repeat procedures.”
- Valderrabano M et al. Abstract 409-12, ACC/WCC 28-30 March 2020.
Posted on
Previous Article
« Non-Alzheimer’s disease pathophysiology in the elderly Next Article
PCI and CABG are equal in left main CAD »
« Non-Alzheimer’s disease pathophysiology in the elderly Next Article
PCI and CABG are equal in left main CAD »
Table of Contents: ACC/WCC 2020
Featured articles
Heart Failure and Cardiomyopathies
Mavacamten shows promising results in non-obstructive hypertrophic cardiomyopathy
Vericiguat shows beneficial effects in a very high-risk HF population
No role for sodium nitrite in out-of-hospital cardiac arrest
Vascular Medicine and Thromboembolism
Rivaroxaban and aspirin effective and safe for PAD patients
TAILOR-PCI misses endpoint but still provides valuable insights
Edoxaban: alternative to warfarin after surgical aortic or mitral valve procedures?
Bleeding reduction post-TAVI with OAC alone vs OAC + clopidogrel
Apixaban offers new perspective for cancer patients in need of anticoagulation
Rivaroxaban superior to enoxaparin in preventing VTE in non-major orthopaedic surgery
Interventional Cardiology
TAVR safe and effective in low-risk bicuspid aortic stenosis patients
TAVR model reveals differences in hospital outcomes
2-year results show non-significant outcomes TAVR vs surgery in severe aortic stenosis
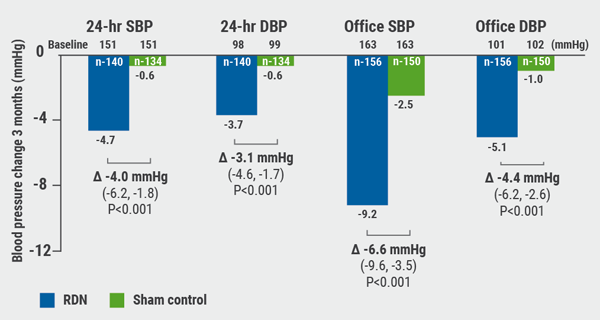
Renal denervation better than sham for blood pressure
Infusion of ethanol in the vein of Marshall for persistent AF
Atrial Fibrillation/Acute Coronary Syndrome
Fewer adverse events with ticagrelor monotherapy after 3 months DAPT
TWILIGHT sub-study: same outcomes for diabetes patients
TWILIGHT sub-study: complex PCI patients
LAAO Watchman registry data positive
Apixaban in AF patients with recent ACS/PCI: Drop aspirin after 30 days
Genetics and Prevention
Homozygous FH responds to alirocumab
Evinacumab significantly reduces LDL-C in homozygous FH patients
Higher serum levels of eicosapentaenoic acid correlate with reduced CV events
Quit smoking: vaping + counselling helps
Related Articles
September 8, 2020
TAVR safe and effective in low-risk bicuspid aortic stenosis patients
September 8, 2020
Renal denervation better than sham for blood pressure
September 8, 2020
Radial artery best for second bypass
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

