In a single-centre study, researchers from the Medical University of Graz (Austria) aimed to assess the clinical impact of the duration of artificial ventilation in stroke patients receiving mechanical thrombectomy under general anaesthesia [1]. They identified all ischaemic stroke patients who had received mechanical thrombectomy for anterior circulation large vessel occlusion under general anaesthesia over a period of 8 years (n=447). Patients were divided into 3 groups, according to ventilation timing: “early” (extubation within 6 hours), “delayed” (6-24 hours), and “late” (>24 hours). The mean age was 69 years, half of patients were female; median ventilation time was 3 hours.
A favourable outcome, defined as modified Rankin Scale scores of 0-2 at 3-months post-stroke, was seen in 188 patients (42.6%) and correlated with shorter ventilation time (P<0.001). In patients extubated ≤24 hours, early extubation was associated with better outcomes than delayed extubation (OR 2.40; 95% CI 1.53-3.76; P<0.001), also in a multivariable analysis (P=0.007). The authors offered a number of possible explanations:
- higher rates of (ventilator-associated) pneumonia;
- impaired cerebral blood flow due possible vasodilatory effects of sedative drugs;
- hyperoxemia, which may occur in ventilated intensive care unit patients;
- delayed early rehabilitation and stroke work-up.
Of 65 patients with late extubation, the most frequent reasons for prolonged intubation were brain oedema (44.6%), impaired consciousness due to other reasons (26.1%), and respiratory insufficiency (15.9%). However, delayed extubations were predicted by non-medical reasons, notably admission outside of core working hours (P<0.001). During neurointensive care, longer ventilation time was strongly associated with a higher rate of pneumonia: 9.6%, 20.6%, and 27.7% in the early, delayed, and late group, respectively (P<0.01).
- Fandler-Höfler S, et al. Abstract O3036, EAN 2020.
Posted on
Previous Article
« Thrombus location and length predictors of early neurological deterioration Next Article
Benefits of statins to prevent stroke outweigh risks »
« Thrombus location and length predictors of early neurological deterioration Next Article
Benefits of statins to prevent stroke outweigh risks »
Table of Contents: EAN 2020
Featured articles
Alzheimer's Disease and Other Dementias
Non-Alzheimer’s disease pathophysiology in the elderly
Novel genetic association with resistance to ERC tau deposition
Diastolic dysfunction novel risk factor for cognitive impairment
Epilepsy
Avoidable epilepsy-related mortality remains high
How genetic testing can contribute to epilepsy management
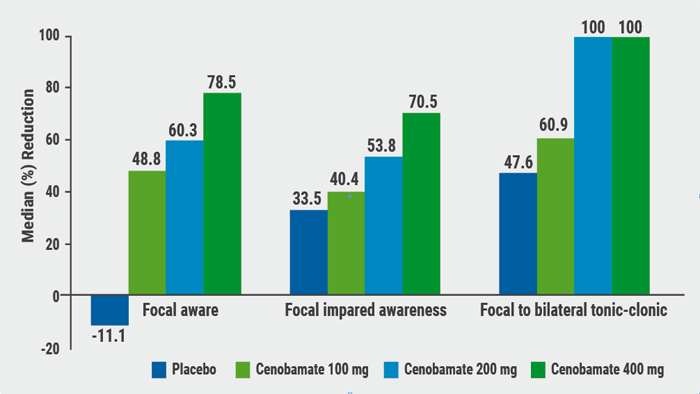
Cenobamate effective in focal epilepsy
Sustained seizure reductions with cannabidiol for Lennox-Gastaut syndrome
Prevalence of autoantibodies in epilepsy almost 10%
Parkinson's Disease
White matter matters in Parkinson’s disease
Sleep disorders mark PD progression
Directional DBS superior to omnidirectional DBS
Stroke
Benefits of statins to prevent stroke outweigh risks
Extubation after thrombectomy: the sooner, the better
Thrombus location and length predictors of early neurological deterioration
Endovascular treatment in large vessel occlusion stroke patients treated with OAC
Early edoxaban may be safe after cardioembolic stroke
Headache and Pain
Small fibre pathology as biomarker for fibromyalgia
Migraine as a cyclical functional disorder
Reassuring real-world safety profile of 3 CGRP inhibitors
Long-term cardiovascular safety of erenumab
Real-world data for erenumab in Germany
Eptinezumab in chronic migraine and medication-overuse headache
Fremanezumab tolerability in cardiovascular patients with migraine
Effects of galcanezumab on health-related quality of life
Multiple Sclerosis
Imaging to evaluate remyelination and neuroprotection
Serum NfL predicts long-term clinical outcomes in MS
Epstein-Barr virus-targeted T-cell immunotherapy for progressive MS
High NEDA rates after 2 years of ocrelizumab
Switching from natalizumab to moderate- versus high-efficacy DMT
Results of compounds in late stages of development
Alemtuzumab efficacy and safety data of over 9 years
Fampridine treatment results in routine clinical practice
Air pollution is a possible risk factor for MS
Neuromyelitis Optica Spectrum Disorder
Genetic association studies in NMOSD needed
Eculizumab in NMOSD: the PREVENT study
Long-term safety of satralizumab consistent with double-blind periods
Neuromuscular Disorders
Biomarkers predicting motor function in SMA
Sustained benefits of avalglucosidase alfa in late-onset Pompe disease
Efficacy and safety of rituximab in refractory MG corroborated
Related Articles
September 8, 2020
Diastolic dysfunction novel risk factor for cognitive impairment
September 9, 2020
Cenobamate effective in focal epilepsy
September 9, 2020
Eptinezumab in chronic migraine and medication-overuse headache
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

