Hydroxychloroquine use is not associated with QTc-length prolongation, even when given in combination with other QTc-prolonging medications. This was demonstrated in an analysis of 681 patients with rheumatic disease.
Hydroxychloroquine (HCQ) plays an essential role in the management of both systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), both as monotherapy and combined with other DMARDs. However, there was an ongoing concern regarding its cardiovascular safety. Recently, the interest increased because of an observational study of COVID-19 patients reporting that 19% of those receiving HCQ demonstrated a QTc >500 ms, including 1 torsades de pointes tachycardia [2]. “Given recent concerns surrounding HCQ use in COVID-19 patients and subsequent arrhythmic events, we wanted to examine the associations between its use and the QTc length on ECG in a large, asymptomatic cohort of RA and SLE patients,” explained study co-author Dr Elizabeth Park (Columbia University Irving Medical Center, USA).
The cross-sectional study analysed data of 681 RA and SLE patients without clinical cardiovascular disease, including 2 prospective RA cohorts of 307 patients and a retrospective SLE cohort of 374 patients. In the 2 prospective RA cohorts, ECGs were performed as part of study data collection, while in the retrospective SLE cohort (n=374) ECGs were performed as part of standard-of-care. Data was adjusted for disease-specific characteristics including prednisone use and cardiovascular disease risk factors.
Of the whole study group (RA and SLE), 54% used HCQ and 44% had QTc lengths of more than 440 ms. The mean QTc length was 437 ± 28 ms. However, in the entire cohort, adjusted QTc length among HCQ users was comparable to those who did not use the drug. In multivariate logistic modelling, HCQ use was not a significant predictor of prolonged QTc. This held true for both the RA and SLE cohort. However, 9 out of 11 of the SLE patients who did have a prolonged QTc were taking HCQ. Yet, these observations were too small to detect statistically significant differences between the HCQ groups.
No significant interactions were found between HCQ and other QTc-prolonging drugs. HCQ use combined with other QTc-prolonging medications resulted in a QTc interval comparable to HCQ alone. In the SLE group, HCQ combined with antipsychotic drugs did result in longer QTc compared with using HCQ alone (441 ms vs 432 ms; P=0.014).
“Overall, the use of HCQ did not predict QTc length, even while adjusting for critical confounding factors, namely the use of other QTc-prolonging medications. Our findings reinforce the fact that HCQ remains a safe, effective long-term disease-modifying drug for our rheumatic disease patients,” Dr Park concluded.
The different results seen in COVID-19 patients might be explained by the fact that these patients were critically ill. Therefore, the effect of COVID-19 itself on the heart and subsequent arrhythmia must be considered.
- Park E. Hydroxychloroquine use was not associated with QTc length in a large cohort of SLE and RA patients. Abstract 0431, ACR Convergence 2020, 5-9 Nov.
- Mercuro NJ, et al. JAMA Cardiol 2020;5:1036-41.
Posted on
Previous Article
« Children with rheumatic disease have no greater risk of a COVID-19 infection Next Article
No elevated risk for influenza AE in tofacitinib-treated RA patients »
« Children with rheumatic disease have no greater risk of a COVID-19 infection Next Article
No elevated risk for influenza AE in tofacitinib-treated RA patients »
Table of Contents: ACR 2020
Featured articles
Late-Breaking News
Gout treatment with febuxostat: no higher cardiovascular mortality
New agent with great potential for the treatment of giant cell arteritis in the pipeline
Autotaxin inhibitor successful in the first trial in diffuse cutaneous systemic sclerosis
JAK inhibition as a treatment option for ankylosing spondylitis
Spotlight on Rheumatoid Arthritis
Persuasive long-term results for JAK inhibition in rheumatoid arthritis
Rheumatoid arthritis: new EULAR treatment guidelines
Rheumatoid arthritis and interstitial lung disease: a deadly combination
COVID-19 – What Rheumatologists Need to Know
COVID-19 in patients with rheumatic disease: most report mild disease
Poor disease control: a risk factor for severe COVID-19
No heightened outcome risk for rheumatic patients with COVID-19
What Is Hot in Lupus Nephritis?
Lupus nephritis biomarkers: moving toward an omic-driven approach
Lupus nephritis: new therapies on the horizon in 2020
Spondyloarthritis – The Beat Goes On
Artificial intelligence can help in the diagnosis of axSPA
Resolution of dactylitis or enthesitis is associated with improvements in joint and skin symptoms
Promising novel treatment option for psoriatic arthritis
How to Diagnose Large Vessel Vasculitis: Promises and Pitfalls
How to choose imaging modalities in large vessel vasculitis
Diagnosis of large vessel vasculitis with imaging
Osteoarthritis – Novel Developments
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate
Anticoagulation with vitamin K antagonist is associated with risk of knee and hip replacement
Osteoporosis – New Data
Bisphosphonate use: Asian American women have a smaller treatment benefit
Inflammatory disease as a risk factor for fractures
Best of the Posters
No progression of osteoarthritis with corticosteroid injections
Hydroxychloroquine use: no indication for arrhythmias in RA and SLE patients
Children with rheumatic disease have no greater risk of a COVID-19 infection
Insufficient antimalarial supply for rheumatic disease treatment in the early COVID-19 pandemic
Related Articles
July 31, 2023
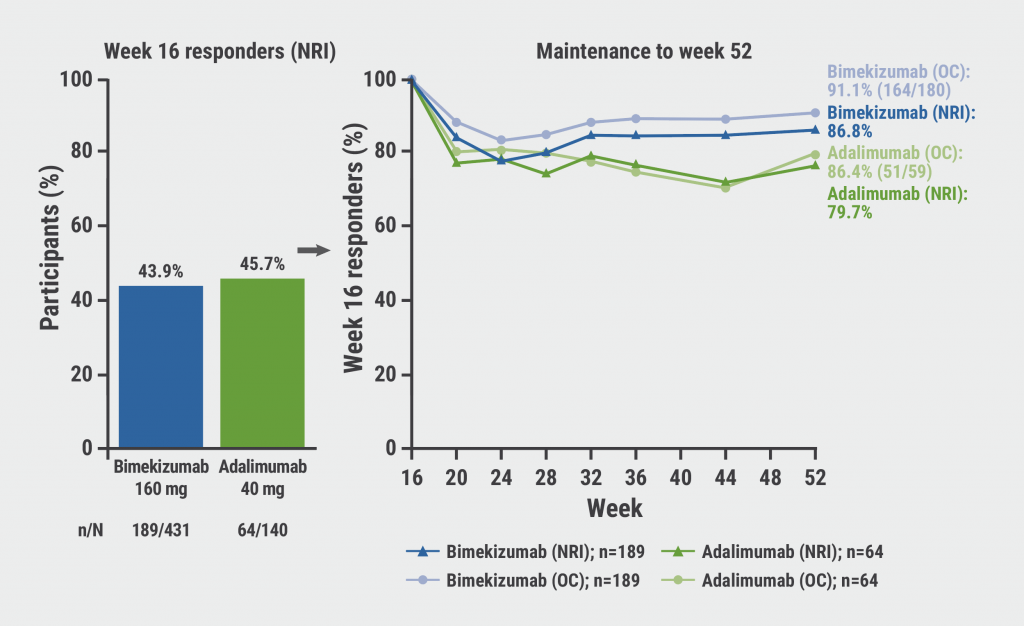
Bimekizumab: high rates of sustained response in PsA
January 14, 2022
More pros than cons for the use of statins in RA
September 29, 2021
Live varicella-zoster vaccine safe, effective with TNF inhibitors
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

