<br>
In contrast to those with direct oral anticoagulation, patients suffering from osteoarthritis using vitamin-K antagonist warfarin had a higher risk of needing knee or hip replacement in a case-control study.
“Currently, we have no disease-modifying treatment available, with joint replacement reserved for end-stage disease,” Dr Priyanka Ballal (Boston University Medical Center, USA) stated concerning osteoarthritis (OA) [1]. She pointed out that vitamin K plays a role in coagulation and that several proteins in bone and cartilage depend on it. “Inadequate levels of vitamin K have been shown to cause abnormal joint tissue mineralisation and contribute to the incidence of OA,” she continued to explain. The current study aimed to find out if antagonising vitamin K by warfarin would increase OA progression.
Using data from The Health Improvement Network, a nested case-control study was performed that included 913 patients with knee and hip replacement. These patients were matched by age and sex to 3,652 controls. This UK database contains medical records from general practitioners and is representative of the general population. Patients were enrolled between 2009 and 2018 and were adults aged 40-80 years that were treated with warfarin or direct oral anticoagulants (DOAC) for atrial fibrillation. Among the exclusion criteria were severe co-morbidities restricting surgery, knee replacement, or hip replacement before 2014 and warfarin or DOAC use within 1 year before the study. By performing a conditional logistic regression, results were controlled for confounders.
Mean age of the study subjects was 75.1 years, 48% were female. Warfarin was given to 64.8% of the cases, while 35.1% received DOAC. Among the controls, the rate of warfarin users was 56.3% and 43.6% received DOAC. The results showed that the confounder-adjusted risk for knee replacement or hip replacement was 57% higher in the warfarin-treated patients (adjusted odds ratio 1.57, 95% CI 1.30–1.89). Compared with DOAC intake, drug exposure to warfarin increased the risk over time. A higher risk was still significant in further adjusted analyses that accounted for other reasons for hip replacement than OA. “We found an incremental risk of hip and knee replacement with the duration of warfarin use,” Dr Ballal further pointed out. In those with warfarin use over 4 years, the risk of requiring hip replacement or knee replacement increased 2-fold (see Figure).
Figure. Gradual increase of risk for hip or knee replacement with the duration of warfarin use [1]

DOAC, direct oral anticoagulants.
“Given the prevalence and impact of OA, our data, along with the existing literature, support the need for a well-powered randomised controlled trial evaluating vitamin K supplementation in OA. Our study also raises the consideration of using DOACs over warfarin when indicated in people with or at risk of OA,” she concluded.
- Ballal P, et al. Warfarin Use and Risk of Knee and Hip Replacements. S0934, ACR Convergence 2020, 5-9 Nov.
Posted on
Previous Article
« Bisphosphonate use: Asian American women have a smaller treatment benefit Next Article
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate »
« Bisphosphonate use: Asian American women have a smaller treatment benefit Next Article
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate »
Table of Contents: ACR 2020
Featured articles
Late-Breaking News
Gout treatment with febuxostat: no higher cardiovascular mortality
New agent with great potential for the treatment of giant cell arteritis in the pipeline
Autotaxin inhibitor successful in the first trial in diffuse cutaneous systemic sclerosis
JAK inhibition as a treatment option for ankylosing spondylitis
Spotlight on Rheumatoid Arthritis
Persuasive long-term results for JAK inhibition in rheumatoid arthritis
Rheumatoid arthritis: new EULAR treatment guidelines
Rheumatoid arthritis and interstitial lung disease: a deadly combination
COVID-19 – What Rheumatologists Need to Know
COVID-19 in patients with rheumatic disease: most report mild disease
Poor disease control: a risk factor for severe COVID-19
No heightened outcome risk for rheumatic patients with COVID-19
What Is Hot in Lupus Nephritis?
Lupus nephritis biomarkers: moving toward an omic-driven approach
Lupus nephritis: new therapies on the horizon in 2020
Spondyloarthritis – The Beat Goes On
Artificial intelligence can help in the diagnosis of axSPA
Resolution of dactylitis or enthesitis is associated with improvements in joint and skin symptoms
Promising novel treatment option for psoriatic arthritis
How to Diagnose Large Vessel Vasculitis: Promises and Pitfalls
How to choose imaging modalities in large vessel vasculitis
Diagnosis of large vessel vasculitis with imaging
Osteoarthritis – Novel Developments
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate
Anticoagulation with vitamin K antagonist is associated with risk of knee and hip replacement
Osteoporosis – New Data
Bisphosphonate use: Asian American women have a smaller treatment benefit
Inflammatory disease as a risk factor for fractures
Best of the Posters
No progression of osteoarthritis with corticosteroid injections
Hydroxychloroquine use: no indication for arrhythmias in RA and SLE patients
Children with rheumatic disease have no greater risk of a COVID-19 infection
Insufficient antimalarial supply for rheumatic disease treatment in the early COVID-19 pandemic
Related Articles
January 18, 2021
No heightened outcome risk for rheumatic patients with COVID-19
September 4, 2019
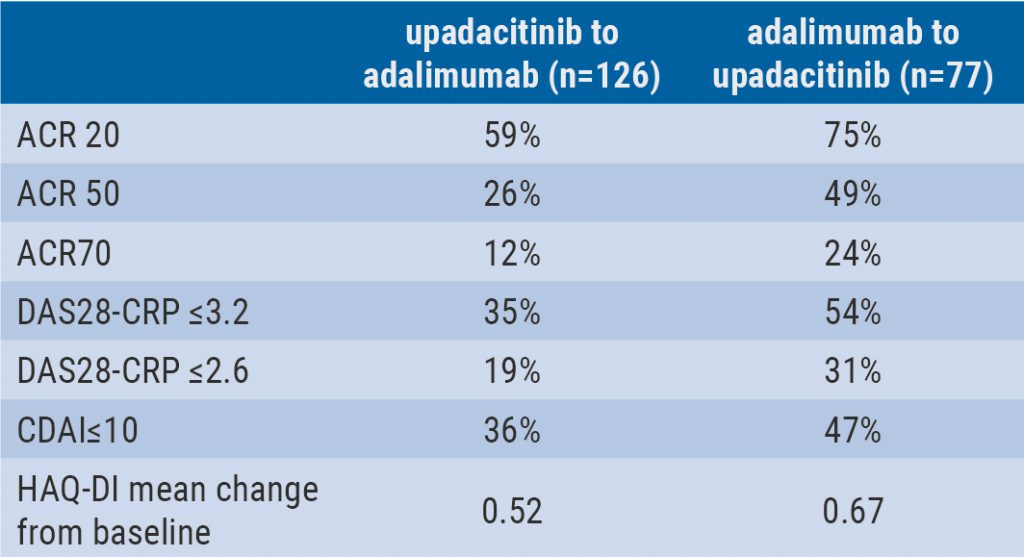
Switching upadacitinib and adalimumab is beneficial in refractory RA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

