In large vessel vasculitis, it is important to understand the limitations of traditional evaluations and to know in what way inflammation may be recognised on different imaging modalities [1]. This talk focused more on the disease entities of Takayasu’s arteritis and giant cell arteritis which share many pathological similarities.
Takayasu’s arteritis is a disease that presents with many different imaging faces. In terms of choosing between the different possible types of angiography that may be performed to diagnose Takayasu’s, Dr Peter Grayson (National Institutes of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), NIH, USA) reflected on several considerations. In general, he rated CT angiography (CTA) and magnetic resonance angiography (MRA) as equivalent. An advantage for the MRA is of course the avoidance of radiation which can be particularly valuable in younger patients. Another aspect to consider in MRA is possible long retention of gadolinium that has been found in different tissues. In any case, Dr Grayson endorsed avoidance of catheter-based angiographies and measurement of central artery pressure in Takayasu’s disease.
The use of temporal artery biopsies (TAB) to diagnose giant cell arteritis (GCA) can also be seen as a medal with 2 sides: on the plus-side, there is tissue-level confirmation, documented findings with a possibility for direct review, and the historically accepted role of TAB as the gold standard. Limitations of TAB include the possibility of missing skip lesions, some cases of CGA in which the temporal arteries are not affected, and the fact that TAB is invasive, expensive, and open to subjective interpretation. Dr Grayson also mentioned that the sensitivity of temporal artery biopsy is declining. He pointed out that large vessel GCA –an increasingly recognised phenotype– may or may not have cranial features of the disease. It includes on one hand less risk for vision loss, but on the other risk for more relapsing and refractory disease. Currently, multi-modal assessment in GCA is being performed in many parts of the world (see Figure). In a large study with 941 GCA patients, 25% had no TAB, 27% of TABs were negative, and 47% positive.
Figure. Use of multi-modal assessments in the diagnosis of GCA [1]
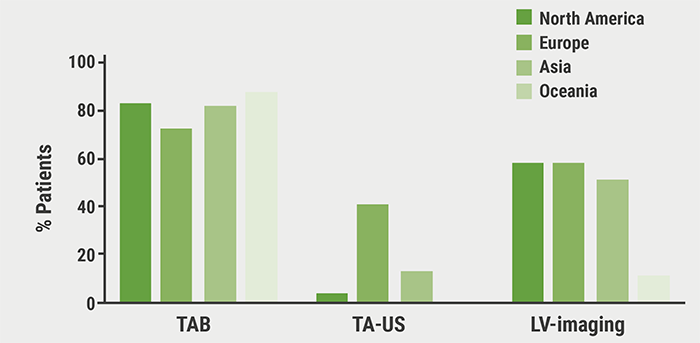
GCA, giant cell arteritis; TAB, temporal artery biopsies; TA-US, temporal artery ultrasound; LV, large vessel.
In summary, Dr Grayson made recommendations for diagnostic imaging in patients with (suspected) GCA, stressing the fact that these were all conditional: TAB is endorsed over temporal artery ultrasound and MRI of cranial arteries. In case of negative biopsy, non-invasive large vessel imaging can aid in diagnosis over clinical assessment alone. Finally, in newly diagnosed GCA, non-invasive vascular imaging can be of help in evaluating large vessel involvement.
- Grayson P. Large Vessel Vasculitis Imaging: Promises and Pitfalls. 2F053, ACR Convergence 2020, 5-9 Nov.
Posted on
Previous Article
« Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate Next Article
How to choose imaging modalities in large vessel vasculitis »
« Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate Next Article
How to choose imaging modalities in large vessel vasculitis »
Table of Contents: ACR 2020
Featured articles
Late-Breaking News
Gout treatment with febuxostat: no higher cardiovascular mortality
New agent with great potential for the treatment of giant cell arteritis in the pipeline
Autotaxin inhibitor successful in the first trial in diffuse cutaneous systemic sclerosis
JAK inhibition as a treatment option for ankylosing spondylitis
Spotlight on Rheumatoid Arthritis
Persuasive long-term results for JAK inhibition in rheumatoid arthritis
Rheumatoid arthritis: new EULAR treatment guidelines
Rheumatoid arthritis and interstitial lung disease: a deadly combination
COVID-19 – What Rheumatologists Need to Know
COVID-19 in patients with rheumatic disease: most report mild disease
Poor disease control: a risk factor for severe COVID-19
No heightened outcome risk for rheumatic patients with COVID-19
What Is Hot in Lupus Nephritis?
Lupus nephritis biomarkers: moving toward an omic-driven approach
Lupus nephritis: new therapies on the horizon in 2020
Spondyloarthritis – The Beat Goes On
Artificial intelligence can help in the diagnosis of axSPA
Resolution of dactylitis or enthesitis is associated with improvements in joint and skin symptoms
Promising novel treatment option for psoriatic arthritis
How to Diagnose Large Vessel Vasculitis: Promises and Pitfalls
How to choose imaging modalities in large vessel vasculitis
Diagnosis of large vessel vasculitis with imaging
Osteoarthritis – Novel Developments
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate
Anticoagulation with vitamin K antagonist is associated with risk of knee and hip replacement
Osteoporosis – New Data
Bisphosphonate use: Asian American women have a smaller treatment benefit
Inflammatory disease as a risk factor for fractures
Best of the Posters
No progression of osteoarthritis with corticosteroid injections
Hydroxychloroquine use: no indication for arrhythmias in RA and SLE patients
Children with rheumatic disease have no greater risk of a COVID-19 infection
Insufficient antimalarial supply for rheumatic disease treatment in the early COVID-19 pandemic
Related Articles
December 1, 2022
Stimulation of PD-1: a new concept to treat RA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

