Vasculopathy, inflammation, and fibrosis form a specific triad of features found in systemic sclerosis (SSc), a disease with a high unmet need for novel treatments. While the pathogenesis of SSc remains uncertain, lysophosphatidic acid (LPA) is a well-known pro-fibrotic and pro-inflammatory lysophospholipid that has been implicated in the pathogenesis of SSc. LPA is generated at sites of inflammation by autotaxin-mediated hydrolysis of lysophosphatidylcholine and other lysophospholipids. Ziritaxestat is an autotaxin inhibitor with a novel mechanism of action that could be promising for modulating the skin pathology of SSc and as such might be able to fill the current treatment gap. The current randomised, double-blind, placebo-controlled phase 2a trial was the first to evaluate oral administration of ziritaxestat in patients with early diffuse cutaneous SSc [1].
Adult patients with diffuse cutaneous SSc (n=33) were randomised 2:1 to receive oral ziritaxestat 600 mg once daily or matching placebo for 24 weeks. Immunosuppressive background therapies were allowed to continue unchanged if doses were stable for ≥3 months prior to ziritaxestat treatment. All patients had a modified Rodnan skin score (mRSS) >10 at screening. The primary endpoint was change from baseline mRSS at 24 weeks. Other endpoints were Health Assessment Questionnaire Disability Index (HAQ-DI) and Combined Response Index for Systemic Sclerosis (ACR CRISS) score. Safety data was collected as well.
The majority of patients in the ziritaxestat (95.2%) and placebo (83.3%) groups were on background immunosuppressive therapy. At baseline, mean (SD) mRSS was 27.0 (8.8) and 22.5 (6.2), respectively. A statistically significant difference was observed between groups for mRSS from week 16 up to week 24: least square mean difference was -2.8 (95% CI -5.6 to -0.1) for ziritaxestat versus placebo (P=0.0411) at week 24. “This effect is significant because this improvement happened despite the background immunosuppressive therapy,” Prof. Dinesh Khanna (University of Michigan Scleroderma Program, USA) explained.
In addition, the ACR CRISS showed likelihood for improvement. Treatment with ziritaxestat did not influence lung function. Target inhibition was reflected by an average reduction in circulating lysophosphatidic acid of about 80%.
Adverse events (AEs) were mild or moderate; no treatment-emergent AE led to study drug discontinuation. Serious treatment-emergent AEs occurred in 2 patients in the ziritaxestat group and 1 patient in the placebo group, all of them were considered unrelated or unlikely to be related to the study drug. “We beleve that these results support a possible role for the autotaxin pathway in early dermal SSc,” Prof. Khanna concluded. This works represents an interesting concept in SSc whereby cutaneous fibrosis may be modulated independently of systemic fibrosis including lung disease. Much interesting exploratory science could flow from these observations.
- Khanna D, et al. A Phase 2a Randomized, Double-blind, Placebo-controlled Study of Ziritaxestat in Early Diffuse Cutaneous Systemic Sclerosis (NOVESA). L09, ACR Convergence 2020, 5-9 Nov.
Posted on
Previous Article
« JAK inhibition as a treatment option for ankylosing spondylitis Next Article
New agent with great potential for the treatment of giant cell arteritis in the pipeline »
« JAK inhibition as a treatment option for ankylosing spondylitis Next Article
New agent with great potential for the treatment of giant cell arteritis in the pipeline »
Table of Contents: ACR 2020
Featured articles
Late-Breaking News
Gout treatment with febuxostat: no higher cardiovascular mortality
New agent with great potential for the treatment of giant cell arteritis in the pipeline
Autotaxin inhibitor successful in the first trial in diffuse cutaneous systemic sclerosis
JAK inhibition as a treatment option for ankylosing spondylitis
Spotlight on Rheumatoid Arthritis
Persuasive long-term results for JAK inhibition in rheumatoid arthritis
Rheumatoid arthritis: new EULAR treatment guidelines
Rheumatoid arthritis and interstitial lung disease: a deadly combination
COVID-19 – What Rheumatologists Need to Know
COVID-19 in patients with rheumatic disease: most report mild disease
Poor disease control: a risk factor for severe COVID-19
No heightened outcome risk for rheumatic patients with COVID-19
What Is Hot in Lupus Nephritis?
Lupus nephritis biomarkers: moving toward an omic-driven approach
Lupus nephritis: new therapies on the horizon in 2020
Spondyloarthritis – The Beat Goes On
Artificial intelligence can help in the diagnosis of axSPA
Resolution of dactylitis or enthesitis is associated with improvements in joint and skin symptoms
Promising novel treatment option for psoriatic arthritis
How to Diagnose Large Vessel Vasculitis: Promises and Pitfalls
How to choose imaging modalities in large vessel vasculitis
Diagnosis of large vessel vasculitis with imaging
Osteoarthritis – Novel Developments
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate
Anticoagulation with vitamin K antagonist is associated with risk of knee and hip replacement
Osteoporosis – New Data
Bisphosphonate use: Asian American women have a smaller treatment benefit
Inflammatory disease as a risk factor for fractures
Best of the Posters
No progression of osteoarthritis with corticosteroid injections
Hydroxychloroquine use: no indication for arrhythmias in RA and SLE patients
Children with rheumatic disease have no greater risk of a COVID-19 infection
Insufficient antimalarial supply for rheumatic disease treatment in the early COVID-19 pandemic
Related Articles
July 31, 2023
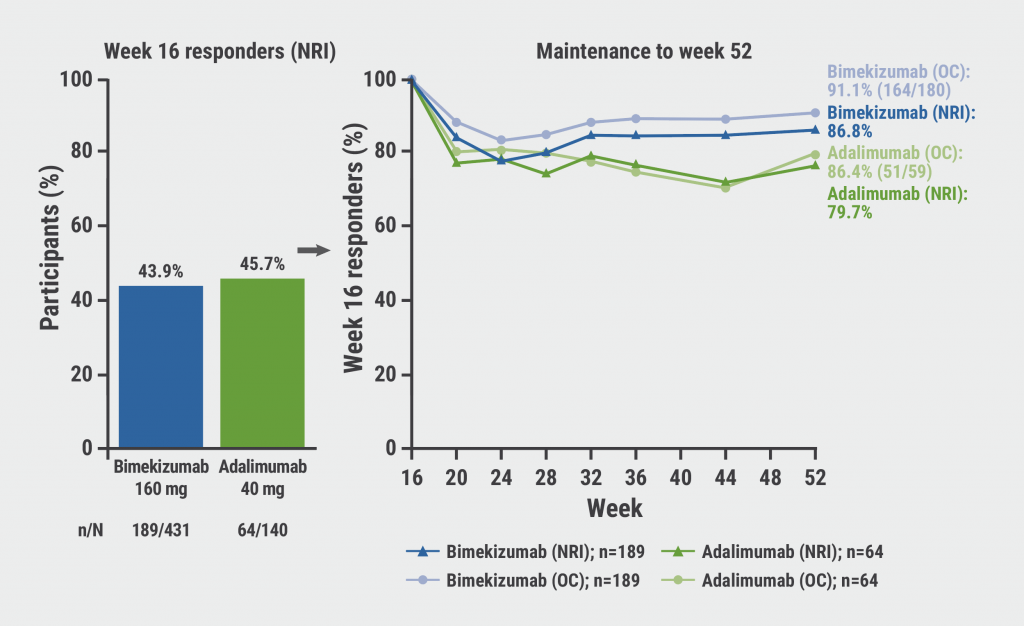
Bimekizumab: high rates of sustained response in PsA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

