https://doi.org/10.55788/b4eb10de
A high prevalence of depressive disorders and links between depression and various long-term outcomes in RA have been observed [1]. “Although antidepressants are used for different indications, we have recently described that, in RA, the most frequent indication for filling antidepressants is depression,” Dr Jens Kristian Pedersen (Odense University Hospital, Denmark) stated [2,3]. The presented cohort study investigated the mortality risk in patients with incident RA and depression [3]. Data was collected from various nationwide Danish registries. The presence of depression was defined as the first filling of an antidepressant prescription. The follow-up period for the all-cause mortality risk was from January 2008 to December 2018. Included in the analysis was data on 11,071 RA patients equalling 56,993 person-years of follow-up.
About 10% of the participants (n=1,095) had a filling of antidepressants during the follow-up period. The median age was 61 years, 66% were women, and 64% had seropositive RA. There was some variance between those with and without exposure to antidepressants. “In those exposed, the age distribution was different, the fraction of women was higher, a lower fraction had seropositive RA, and the median Health Assessment Questionnaire Disability Index (HAQ) and Disease Activity Score-28 (DAS28) were higher than in those not exposed,” Dr Pedersen pointed out.
The results of the adjusted analysis for mortality hazard in RA patients with or without depression revealed the highest risk for exposed patients under the age of 55 years (HR 6.66; 95% CI 2.80–15.85). Corresponding HR for the other age groups receiving antidepressants were 3.3 for 55–70 years and 2.94 for >70 years old. Mortality was increased by depression in men (HR 3.70) and women (HR 2.91), as well as seropositive (HR 3.45) and seronegative RA (HR 3.08). “According to exposure status (to antidepressants), the cumulative mortality followed 2 clearly different paths: the mortality curves separated early and already within the first and second year of follow-up,” Dr Pedersen commented on the Kaplan-Meier curves for exposed and non-exposed participants.
- Matcham F, et al. Rheumatology. 2013;52:2136–2148.
- Pedersen JK, et al. Scand J Rheumatol. 2022;51:173–179.
- Pedersen JK, et al. More than six-fold increased mortality risk in patients with incident rheumatoid arthritis and depression in a large cohort with 10-year follow-up. OP0067, EULAR 2022 Congress, 1-4 June, Copenhagen, Denmark.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Preventive treatment with methotrexate benefits pre-RA patients with arthralgia Next Article
Many RA and PsA patients have problems with their sex life »
« Preventive treatment with methotrexate benefits pre-RA patients with arthralgia Next Article
Many RA and PsA patients have problems with their sex life »
Table of Contents: EULAR 2022
Featured articles
Late-Breaking Oral Abstracts
TYK2 inhibition: the future of treating lupus erythematosus?
Psoriatic arthritis: significant improvement with bimekizumab
Baricitinib could open the door to oral treatment for juvenile idiopathic arthritis
Sarilumab for polymyalgia rheumatica led to sustained remission and fewer flares
Spotlight on Rheumatoid Arthritis
Comorbid depression comes with a profoundly higher mortality risk in RA
Preventive treatment with methotrexate benefits pre-RA patients with arthralgia
Risk factors for dementia in RA patients discovered
VTE in global registry data more common in JAK inhibitor-treated RA patients
Spondyloarthropathies – Novel Developments
How to treat enthesitis in 2022
Baseline cardiovascular risk linked to higher rates of MACE in PsA and PsO patients receiving tofacitinib
Treat-to-target dose reduction effective in spondyloarthritis
A novel oral treatment possibility for non-radiographic axSpA on the horizon
Many RA and PsA patients have problems with their sex life
What Is Hot in Osteoarthritis?
New treatments in osteoarthritis
OA associated with alcohol and drug abuse
Body mass index increase associated with structural changes in knee OA
What Is New in Lupus and Scleroderma
Inhibition of Bruton’s tyrosine kinase: a new way of approaching SLE?
Pregnancies in SLE: many complications for mothers and their unborn children
Lupus nephritis: Efficient treatment may reduce the risk of kidney disease advancement
Antifibrotic therapy with nintedanib is beneficial for patients with negative prognostic factors
Best of the Posters
Alarmingly low activity in patients with non-inflammatory and inflammatory rheumatic disease
High prevalence of fibromyalgia in patients with inflammatory bowel disease
Related Articles
January 29, 2021
Cigarette smoke tied to colorectal neoplasia in IBD patients
May 9, 2019
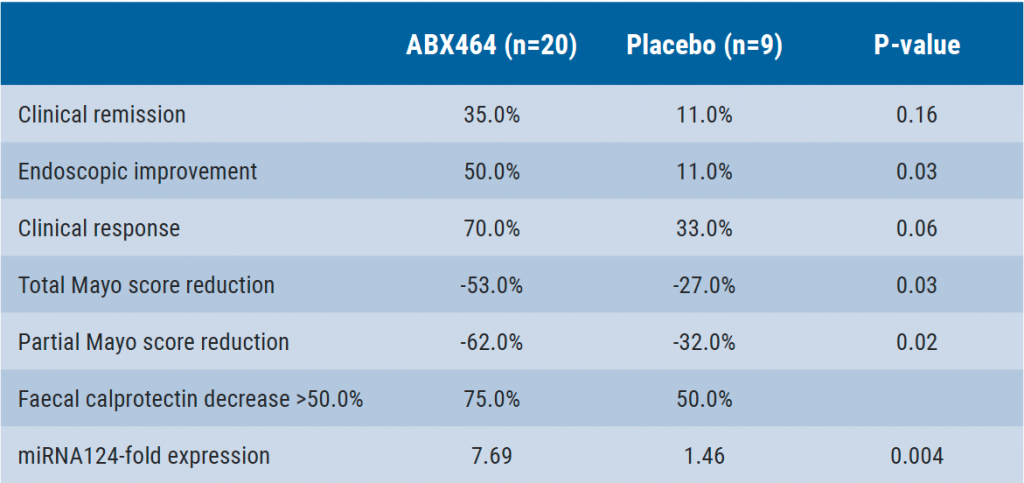
ABX464: HIV drug tested in ulcerative colitis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

