https://doi.org/10.55788/0444ff67
“After transplantation, we know that patients who have undergone a colectomy have decreased rates of recurrent PSC and also a better graft survival,” Dr Bregje Mol (Amsterdam UMC, the Netherlands) said [1]. Since the effect of colectomy before transplantation remains unclear to date, Dr Mol and colleagues conducted a retrospective cohort study to explore the effect of proctocolectomy with ileostomy on transplant-free survival in patients with PSC. “The studies that are available either consist of small patient numbers, don’t take known risk factors into account, or sometimes don’t take colectomy into account as a time-dependent variable,” Dr Mol explained. The present study did introduce colectomy as a time-dependent variable. The analysis also corrected for known risk factors like age, sex, concomitant IBD or autoimmune hepatitis, and enrolment in a tertiary centre of care.
The trial enrolled 1,341 adult patients from the EpiPSC2 cohort between 2008 and 2021, leading to over 14,000 patient-years of follow-up. The mean age at PSC diagnosis was 39 years and 36% were women. Most patients had large-duct PSC (86%) and 68% had been diagnosed with IBD. Most of the observed colectomies were indicated by dysplasia/neoplasia or active colitis. During follow-up, the median transplant-free survival was about 19 years.
“We observed 370 liver transplants and almost 400 deaths, of which PSC-related deaths were most common,” Dr Mol stated. Comparison between no colectomy, colectomy with remnant colon, or proctocolectomy with ileostomy showed a protective effect of proctocolectomy with ileostomy regarding liver transplantation and PSC-related death (HR 0.47; 95% CI 0.24–0.93; see Figure). For other forms of colectomy with residual colon, no benefit was found. Interestingly, the IBD status of the participants had no impact.
Figure: Results of patients with primary sclerosing cholangitis undergoing no colectomy, colectomy with remnant colon, or proctocolectomy with ileostomy [1]
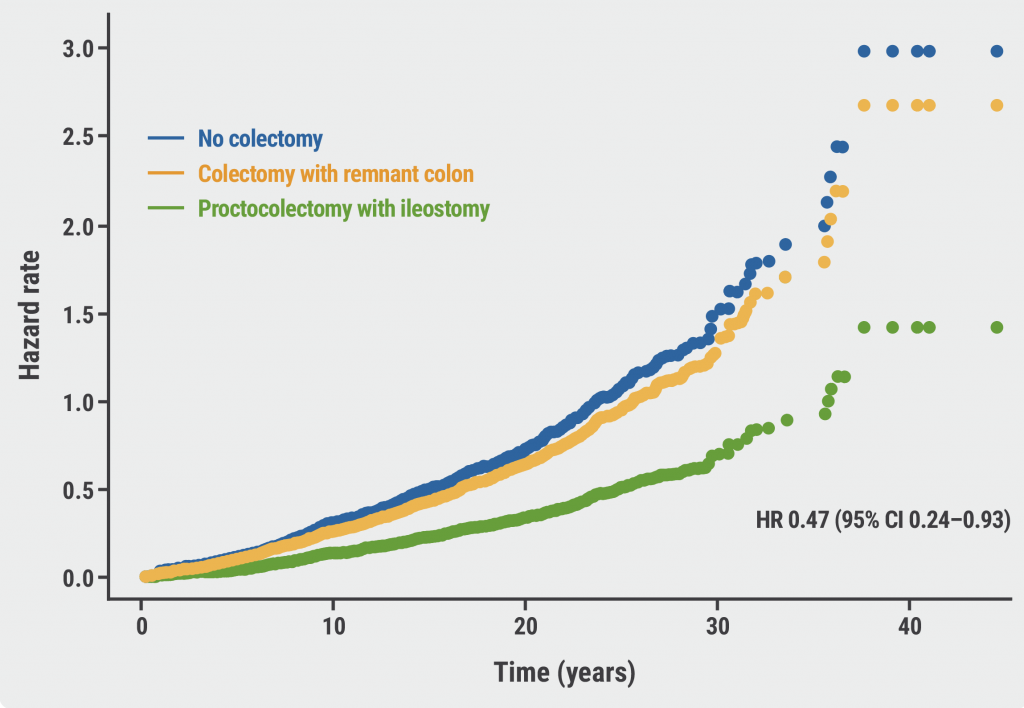
“In our data, proctocolectomy with ileostomy seems to be associated with a better transplant-free survival, which points towards a role for the colonic microbiota in the disease course of PSC. You only see this effect when you perform a colectomy with ileostomy, so no colonic microbiota can remain, and this effect was not seen with any remnant colon function,” Dr Mol concluded.
- Mol B, et al. Proctocolectomy with permanent ileostomy is associated with better transplant-free survival in patients with primary sclerosing cholangitis: a retrospective cohort study. LB02, UEG Week 2022, 8–11 October, Vienna, Austria.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« SARS-CoV-2: Booster doses of key importance for cirrhotic patients Next Article
Portal hypertension is associated with poor prognosis in cirrhotic patients »
« SARS-CoV-2: Booster doses of key importance for cirrhotic patients Next Article
Portal hypertension is associated with poor prognosis in cirrhotic patients »
Table of Contents: UEGW 2022
Featured articles
IBD in 2022
Fast recapture of response with ozanimod after withdrawal in UC
Ozanimod treatment prompted substantial response after failure of response to induction
Etrasimod shows advantage over placebo in UC
Etrasimod reduces adaptive immune cells in the periphery in UC
Favourable maintenance rates for risankizumab also in delayed responders with CD
IL-23 inhibition reduces inflammatory biomarkers in pre-treated UC
Maintained symptom control with mirikizumab in UC
Mirikizumab successfully resolves active histologic inflammation in UC
Upadacitinib for CD: remarkable efficacy in induction therapy
Sustained maintenance results with upadacitinib in UC
Another chance for TYK2 inhibition in UC
Small molecule obefazimod shows promise in UC
Pivotal results of etrolizumab for CD partly disappointing
Better results for vedolizumab in early CD
Some patients with limited CD may benefit from an early surgical intervention
Dose-interval of adalimumab might be prolonged in CD patients in stable remission
What Is Hot in Upper GI Disorders?
Less ulcer bleeds early after H. pylori eradication in aspirin users
Dupilumab effective in paediatric patients with eosinophilic oesophagitis
Neoplasia in Barrett’s oesophagus: the earlier the intervention, the better the long-term outcome
Hepatology in 2022
Favourable pancreatitis outcomes with procalcitonin-based algorithm to guide antibiotic use
Portal hypertension is associated with poor prognosis in cirrhotic patients
Chances of transplant-free survival in PSC enhanced by colectomy with ileostomy
SARS-CoV-2: Booster doses of key importance for cirrhotic patients
What Is New in Pancreatic Cancer and Pancreatitis?
Fewer long-term interventions after delayed drainage in necrotising pancreatitis
Detection of Europe´s deadliest cancer: much room for improvement
Colorectal Carcinoma: Improving Diagnosis and Therapy
Immunotherapy response may be modulated by microbiome
Computer-aided colonoscopies improved adenoma detection rates
Screening-detected colorectal cancers may have superior surgical outcomes
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com