Prof. Michael Böhm (Saarland University Medical Center, Germany) presented the international, prospective, single-blinded, sham-controlled trial, which was designed to assess the efficacy of renal denervation in the absence of antihypertensive medications [1]. The findings were simultaneously published in The Lancet [2].
This trial was instigated based on observational data suggesting that catheter-based renal denervation significantly reduced blood pressure. Following a positive pilot trial, the SPYRAL PIVOTAL-SPYRAL HTN-OFF MED trial was powered to evaluate the efficacy of catheter-based renal denervation in the absence of medications. Participants (n=331) from 46 sites had a systolic blood pressure (average over 24 hours) between 140 -170 mmHg and had either never taken any blood pressure-reducing medications or had discontinued those medications for at least 3 weeks prior to study entry. Characteristics were similar between both groups; 67% were men, the average age was 53, and the average body mass index was 31. Patients were randomised to either renal denervation (n=166) or a sham procedure (n=165), during which a catheter was inserted and angiography was performed.
The primary efficacy endpoint was the change in average 24-hour systolic blood pressure at 3 months post-procedure, adjusted for systolic blood pressure at study entry. The secondary efficacy endpoint was the change in average blood pressure measured in the doctor’s office at 3 months, adjusted for office blood pressure at study entry. Major adverse safety events were also assessed at 3 months, including rates of death, stroke, changes in kidney function, or any injury to the arteries surrounding the kidney.
Both endpoints were met. At 3 months, a significant 4.7 mmHg reduction was observed in patients’ 24-hour systolic ambulatory blood pressure and a 9.2 mmHg reduction in office systolic blood pressure. Change in 24-hour systolic blood pressure was 3.9 mmHg (P<0.001) and change in office systolic blood pressure at was 6.6 mmHg (P<0.001; see Figure). No deaths, strokes, or decreases in kidney function occurred during the first 3-months of follow-up.
Figure: Primary analysis of blood pressure at 3 months over 24-hours at home or the office [1]
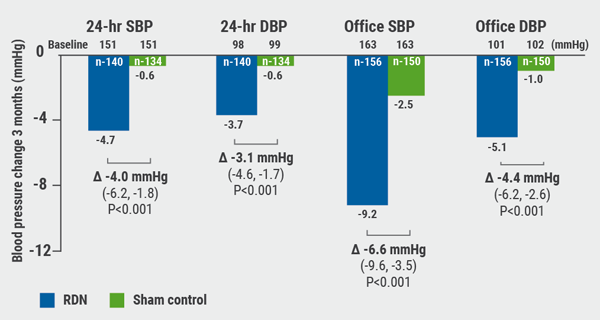
DBP, diastolic blood pressure; RDN, renal denervation; SBP, systolic blood pressure. Figure kindly provided by Prof. Blöm.
Prof. Böhm concluded: “The findings show that renal denervation lowers blood pressure not just during the day but also through the night and early morning periods when risk is highest for clinical events and the effect of some medications on blood pressure is reduced. This study establishes renal denervation as an additional option beyond exercise or lifestyle modification for patients with high blood pressure who are unwilling to take or cannot tolerate medication.”
Results from a companion study, the SPYRAL HTN-ON MED trial, which is testing the safety and effectiveness of renal denervation in patients who are taking up to 3 blood pressure-reducing medications, are expected at the end of 2021.
- Böhm M, et al. Abstract 406-15. ACC/WCC 28-30 March 2020.
- Böhm M, et al. Lancet 2020;Mar 29. doi: 1016/S0140-6736(20)30554-7.
Posted on
Previous Article
« Radial artery best for second bypass Next Article
2-year results show non-significant outcomes TAVR vs surgery in severe aortic stenosis »
« Radial artery best for second bypass Next Article
2-year results show non-significant outcomes TAVR vs surgery in severe aortic stenosis »
Table of Contents: ACC/WCC 2020
Featured articles
Heart Failure and Cardiomyopathies
Mavacamten shows promising results in non-obstructive hypertrophic cardiomyopathy
Vericiguat shows beneficial effects in a very high-risk HF population
No role for sodium nitrite in out-of-hospital cardiac arrest
Vascular Medicine and Thromboembolism
Rivaroxaban and aspirin effective and safe for PAD patients
TAILOR-PCI misses endpoint but still provides valuable insights
Edoxaban: alternative to warfarin after surgical aortic or mitral valve procedures?
Bleeding reduction post-TAVI with OAC alone vs OAC + clopidogrel
Apixaban offers new perspective for cancer patients in need of anticoagulation
Rivaroxaban superior to enoxaparin in preventing VTE in non-major orthopaedic surgery
Interventional Cardiology
TAVR safe and effective in low-risk bicuspid aortic stenosis patients
TAVR model reveals differences in hospital outcomes
2-year results show non-significant outcomes TAVR vs surgery in severe aortic stenosis
Renal denervation better than sham for blood pressure
Infusion of ethanol in the vein of Marshall for persistent AF
Atrial Fibrillation/Acute Coronary Syndrome
Fewer adverse events with ticagrelor monotherapy after 3 months DAPT
TWILIGHT sub-study: same outcomes for diabetes patients
TWILIGHT sub-study: complex PCI patients
LAAO Watchman registry data positive
Apixaban in AF patients with recent ACS/PCI: Drop aspirin after 30 days
Genetics and Prevention
Homozygous FH responds to alirocumab
Evinacumab significantly reduces LDL-C in homozygous FH patients
Higher serum levels of eicosapentaenoic acid correlate with reduced CV events
Quit smoking: vaping + counselling helps
Related Articles
September 8, 2020
TAVR safe and effective in low-risk bicuspid aortic stenosis patients
September 8, 2020
TWILIGHT sub-study: same outcomes for diabetes patients
September 8, 2020
Radial artery best for second bypass
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

