Prof. Michael Mack (Baylor Scott & White Heart Hospital, USA) presented the 2-year clinical and echocardiographic outcomes of the PARTNER 3 trial for low-risk patients with severe symptomatic aortic stenosis who were treated with the SAPIEN 3 TAVR system compared with surgery. A thousand patients were randomised 1:1 to TAVR and surgery; follow-up was done at 30 days, 6 months, and continuing annually through 10 years. The primary endpoint was a composite of all-cause mortality, stroke, or CV rehospitalisation at 1 year post-procedure. Participants had severe calcific aortic stenosis and low surgical risk, mean age was 73 years, and mean Society of Thoracic Surgeons (STS) score was 1.9. At 2 years, 96.5% of participants were available for primary endpoint analysis.
At 1 year, a primary endpoint event occurred in 15.6% of surgery patients and in 8.5% of TAVR patients; at 2 years, these numbers rose to 17.4% versus 11.5%, respectively. Death at 1 year occurred in 2.5% of surgery patients versus 1.0% of TAVR patients; at 2 years, this was 3.2% and 2.4%, respectively. The rates for stroke at 1 year were 3.3% and 1.2%, respectively, and 3.6% versus 2.4% at 2 years. The results were complex; because the patients experienced more CV events/deaths between 1-2 years, the benefits were offset by 2 years. At 1 year, the incidence of new-onset atrial fibrillation was lower in the TAVR arm (7.9% vs 41.8%; P<0.001) and the incidence of new-onset left bundle branch block was higher (24.4% vs 9.4%; P<0.001). Likewise, at 2 years, 2.6% of TAVR patients had valve thrombosis compared with 0.7% of surgery patients (P=0.02).
Limitations of the study included that the results only apply to the enrolled selected population, which excluded a large number of patients. Also, there was less follow-up data available in the surgical group as more patients withdrew from the study. Finally, it was pointed out that valve thrombosis definitions by Valve Academic Research Consortium (VARC) 2 criteria are outdated and may be exaggerated by recent CT imaging leaflet thickening studies, and that results reflect only 2-year outcomes, which makes long-term assessment of structural valve deterioration necessary.
Prof. Mack concluded that the main take-home messages were “that there are 2 good options for low-risk patients and that there should be shared decision-making with the patient as to which option is best for them.” He pointed out that PARTNER 3 was not an all-comers trial, “so if you put it in that framework and have patients who were studied in the trial, both options are good options based upon 2-year data. However, extending the findings of this trial to the population outside of that study is a bridge too far.”
- Leon MB, et al. Abstract 405-16. ACC/WCC 28-30 March 2020.
Posted on
Previous Article
« Renal denervation better than sham for blood pressure Next Article
Real-world evidence for MitraClip »
« Renal denervation better than sham for blood pressure Next Article
Real-world evidence for MitraClip »
Table of Contents: ACC/WCC 2020
Featured articles
Heart Failure and Cardiomyopathies
Mavacamten shows promising results in non-obstructive hypertrophic cardiomyopathy
Vericiguat shows beneficial effects in a very high-risk HF population
No role for sodium nitrite in out-of-hospital cardiac arrest
Vascular Medicine and Thromboembolism
Rivaroxaban and aspirin effective and safe for PAD patients
TAILOR-PCI misses endpoint but still provides valuable insights
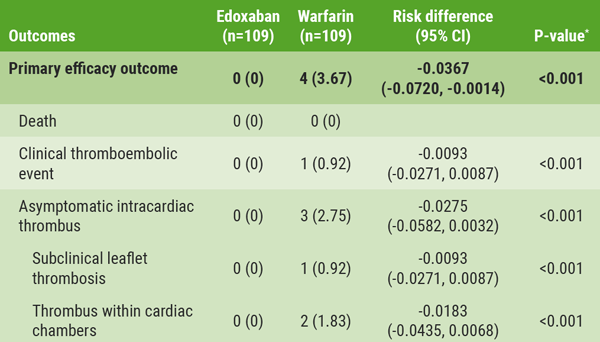
Edoxaban: alternative to warfarin after surgical aortic or mitral valve procedures?
Bleeding reduction post-TAVI with OAC alone vs OAC + clopidogrel
Apixaban offers new perspective for cancer patients in need of anticoagulation
Rivaroxaban superior to enoxaparin in preventing VTE in non-major orthopaedic surgery
Interventional Cardiology
TAVR safe and effective in low-risk bicuspid aortic stenosis patients
TAVR model reveals differences in hospital outcomes
2-year results show non-significant outcomes TAVR vs surgery in severe aortic stenosis
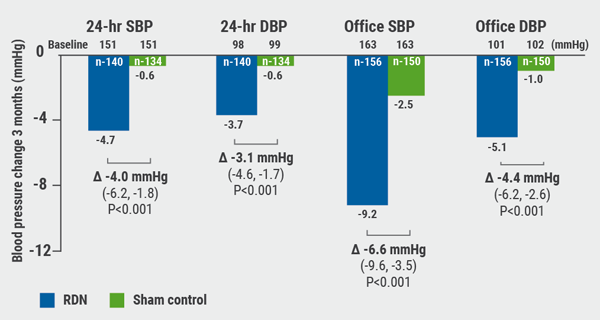
Renal denervation better than sham for blood pressure
Infusion of ethanol in the vein of Marshall for persistent AF
Atrial Fibrillation/Acute Coronary Syndrome
Fewer adverse events with ticagrelor monotherapy after 3 months DAPT
TWILIGHT sub-study: same outcomes for diabetes patients
TWILIGHT sub-study: complex PCI patients
LAAO Watchman registry data positive
Apixaban in AF patients with recent ACS/PCI: Drop aspirin after 30 days
Genetics and Prevention
Homozygous FH responds to alirocumab
Evinacumab significantly reduces LDL-C in homozygous FH patients
Higher serum levels of eicosapentaenoic acid correlate with reduced CV events
Quit smoking: vaping + counselling helps
Related Articles
September 8, 2020
Renal denervation better than sham for blood pressure
September 8, 2020
Real-world evidence for MitraClip
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

