Presenting the first large trial to address the added value of e-cigarettes for smoking cessation, Prof. Mark J. Eisenberg (McGill University, Canada) described The Evaluating the Efficacy of E-Cigarette Use for Smoking Cessation E3 study [1]. The trial randomly assigned participants to receive nicotine e-cigarettes and minimal counselling, non-nicotine e-cigarettes and minimal counselling, or only minimal counselling for 12 weeks. Participants will be followed for 1 year to see which (if any) group is more likely to have quit or reduced their cigarette consumption. The primary outcome measure was the 7-day prevalence of self-reported smoking abstinence at 12 weeks, coupled with a measurement of exhaled carbon monoxide less than 11 ppm.
E3 enrolled 376 people (mean age 52 years; 53% men) at 17 sites in Canada. On average, these individuals had smoked 21 cigarettes a day for the previous 35 years. Of the participants, 91% had tried to quit smoking before but had failed. Most had already tried smoking cessation medications or behavioural therapy; about 1/3 had previously tried e-cigarettes.
All participants received 100 minutes of smoking cessation counselling over the 12-week study period. Participants self-reported their progress during 3 phone calls. Twice during the 12 weeks, they visited a clinic to undergo a breath test for carbon monoxide to confirm smoking behaviour.
In the nicotine e-cigarette group, there was a 12.8% absolute difference in 12-week quit rates compared with counselling alone (relative risk [RR] 2.4; 95% CI 1.3-4.6). The e-cigarette group without nicotine was 8.2% more likely to quit than the counselling group, which was not quite a significant difference (RR 1.9; 95% CI 1.0-3.8).
No adverse events were noted, except for 1 patient in the nicotine e-cigarette group whose pre-existing chronic pulmonary disease worsened.
Because of a manufacturing delay in the e-cigarettes, the researchers halted enrolment at 77% of their target. To compensate for the reduced statistical power, the study had to change its planned primary endpoint from 52-week follow-up, to only analysing the end of the 12-week treatment period. Six- and 12-month data are still forthcoming and will help determine the long-term effect of the intervention and whether it promotes permanent cessation.
- Eisenberg MJ, et al. Abstract 11-08. ACC/WCC 28-30 March 2020.
Posted on
Previous Article
« TAVR safe and effective in low-risk bicuspid aortic stenosis patients Next Article
Adjuvant osimertinib in NSCLC: practice changing ADAURA trial »
« TAVR safe and effective in low-risk bicuspid aortic stenosis patients Next Article
Adjuvant osimertinib in NSCLC: practice changing ADAURA trial »
Table of Contents: ACC/WCC 2020
Featured articles
Heart Failure and Cardiomyopathies
Mavacamten shows promising results in non-obstructive hypertrophic cardiomyopathy
Vericiguat shows beneficial effects in a very high-risk HF population
No role for sodium nitrite in out-of-hospital cardiac arrest
Vascular Medicine and Thromboembolism
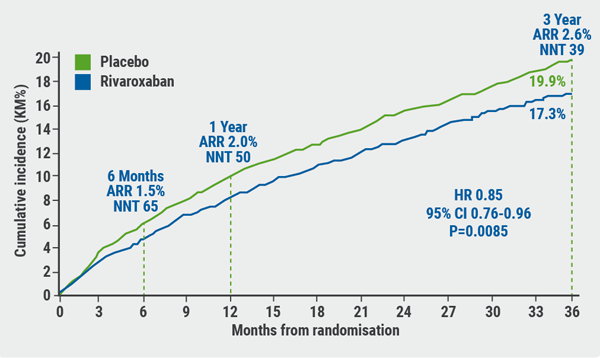
Rivaroxaban and aspirin effective and safe for PAD patients
TAILOR-PCI misses endpoint but still provides valuable insights
Edoxaban: alternative to warfarin after surgical aortic or mitral valve procedures?
Bleeding reduction post-TAVI with OAC alone vs OAC + clopidogrel
Apixaban offers new perspective for cancer patients in need of anticoagulation
Rivaroxaban superior to enoxaparin in preventing VTE in non-major orthopaedic surgery
Interventional Cardiology
TAVR safe and effective in low-risk bicuspid aortic stenosis patients
TAVR model reveals differences in hospital outcomes
2-year results show non-significant outcomes TAVR vs surgery in severe aortic stenosis
Renal denervation better than sham for blood pressure
Infusion of ethanol in the vein of Marshall for persistent AF
Atrial Fibrillation/Acute Coronary Syndrome
Fewer adverse events with ticagrelor monotherapy after 3 months DAPT
TWILIGHT sub-study: same outcomes for diabetes patients
TWILIGHT sub-study: complex PCI patients
LAAO Watchman registry data positive
Apixaban in AF patients with recent ACS/PCI: Drop aspirin after 30 days
Genetics and Prevention
Homozygous FH responds to alirocumab
Evinacumab significantly reduces LDL-C in homozygous FH patients
Higher serum levels of eicosapentaenoic acid correlate with reduced CV events
Quit smoking: vaping + counselling helps
Related Articles
September 7, 2020
Rivaroxaban and aspirin effective and safe for PAD patients
September 8, 2020
Infusion of ethanol in the vein of Marshall for persistent AF
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

