The new EULAR guidelines on the management of rheumatoid arthritis (RA) were presented by Prof. Daniel Aletaha (Medical University Vienna, Austria) [1,2]. His presentation covered the following topics: treat-to-target and remission, precision medicine, expanding therapeutic opportunities, glucocorticoids, and possible treatment reduction decisions [1].
The treat-to-target approach has been widely implemented among rheumatologists for about 10 years. Remission criteria are not new, but recently, there has been some discussion on the role of Patient Global Assessment (PGA) within the Boolean criteria. There is ongoing research about the use of increasing the cut-off point for the PGA to improve the consistency of the Boolean criteria with the Simple Disease Activity Index (SDAI) criteria.
Regarding precision medicine, Prof. Aletaha indicated that, currently, there are no single or combined markers that drive treatment guidance for RA patients at baseline to tailor biologic treatment. “The problem is that often only one therapy is investigated based on clinical trials that are analysed. Often we only look at “-omics” and we should be thinking about a broader context, maybe going to socio-demographics and age, or other factors that –combined with biological data– can create a biotype that can then be used to try and predict a phenotype. These markers will then give you the precision-medicine approach,” Prof. Aletaha elaborated. Hence, the challenges of precision medicine might be partly due to the heterogeneity of outcome and the lack of phenotypes of response.
JAK Inhibitors: a novel addition in the guidelines
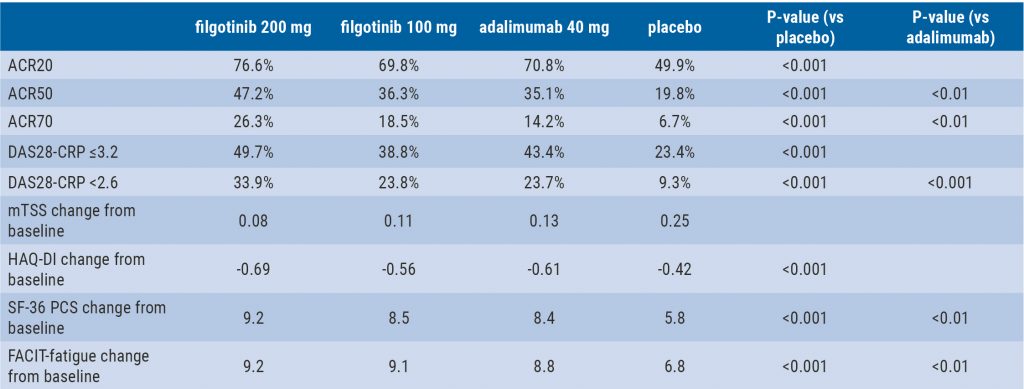
The EULAR recommendations newly implemented JAK inhibitors on the same level as biologic DMARDs after failure of methotrexate (see Figure). Concerning small molecules, Prof. Aletaha recapitulated that the targeted synthetics approach various targets while biologics are highly efficient for one specific target and may indirectly target others.
Figure. New position of JAK inhibition in the EULAR 2020 recommendations [2]

RF, rheumatoid factor; ACPA, anticitrullinated protein antibody; DMARDs, disease-modifying antirheumatic drugs; csDMARDs, conventional synthetic DMARDs; bDMARD, biologic DMARD.
As for glucocorticoids: they should be combined short term with conventional DMARDs. This is partly based on outcomes from the IDEA study [3]. In IDEA, methotrexate plus infliximab had no statistically significant superiority over methotrexate plus high-dose corticosteroids in DMARD-naïve early RA patients. Furthermore, the NORD-STAR trial (NCT01491815) assessed aggressive conventional therapy including corticosteroids and the results showed that it had relative non-inferiority compared with other treatments like biologics [4].
The last subject covered was medication tapering for patients who reached their treatment target recommended by the current EULAR algorithm [1]. “The most important question when we want to taper off patients on biological DMARDs is: which predictors are indicating successful discontinuation,“ said Prof. Aletaha. He indicated that these include low disease activity, better physical function, absence or low presence of rheumatoid factor (RF) or anticitrullinated protein antibody (ACPA), low levels of C-reactive protein (CRP), shorter disease duration, and low signals of disease activity by ultrasound.
- Aletaha D. In 2020, what recent data guide treatment decisions in rheumatoid arthritis? 4S005, ACR Convergence 2020, 5-9 Nov.
- Smolen JS, et al. Ann Rheum Dis. 2020;79:685-99.
- Nam JL, et al. Ann Rheum Dis. 2014;73:75-85.
- Hetland ML, et al. L09, 2019 ACR/ARP Annual Meeting.
Posted on
Previous Article
« Rheumatoid arthritis and interstitial lung disease: a deadly combination Next Article
Persuasive long-term results for JAK inhibition in rheumatoid arthritis »
« Rheumatoid arthritis and interstitial lung disease: a deadly combination Next Article
Persuasive long-term results for JAK inhibition in rheumatoid arthritis »
Table of Contents: ACR 2020
Featured articles
Late-Breaking News
Gout treatment with febuxostat: no higher cardiovascular mortality
New agent with great potential for the treatment of giant cell arteritis in the pipeline
Autotaxin inhibitor successful in the first trial in diffuse cutaneous systemic sclerosis
JAK inhibition as a treatment option for ankylosing spondylitis
Spotlight on Rheumatoid Arthritis
Persuasive long-term results for JAK inhibition in rheumatoid arthritis
Rheumatoid arthritis: new EULAR treatment guidelines
Rheumatoid arthritis and interstitial lung disease: a deadly combination
COVID-19 – What Rheumatologists Need to Know
COVID-19 in patients with rheumatic disease: most report mild disease
Poor disease control: a risk factor for severe COVID-19
No heightened outcome risk for rheumatic patients with COVID-19
What Is Hot in Lupus Nephritis?
Lupus nephritis biomarkers: moving toward an omic-driven approach
Lupus nephritis: new therapies on the horizon in 2020
Spondyloarthritis – The Beat Goes On
Artificial intelligence can help in the diagnosis of axSPA
Resolution of dactylitis or enthesitis is associated with improvements in joint and skin symptoms
Promising novel treatment option for psoriatic arthritis
How to Diagnose Large Vessel Vasculitis: Promises and Pitfalls
How to choose imaging modalities in large vessel vasculitis
Diagnosis of large vessel vasculitis with imaging
Osteoarthritis – Novel Developments
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate
Anticoagulation with vitamin K antagonist is associated with risk of knee and hip replacement
Osteoporosis – New Data
Bisphosphonate use: Asian American women have a smaller treatment benefit
Inflammatory disease as a risk factor for fractures
Best of the Posters
No progression of osteoarthritis with corticosteroid injections
Hydroxychloroquine use: no indication for arrhythmias in RA and SLE patients
Children with rheumatic disease have no greater risk of a COVID-19 infection
Insufficient antimalarial supply for rheumatic disease treatment in the early COVID-19 pandemic
Related Articles
December 1, 2022
Stimulation of PD-1: a new concept to treat RA
January 17, 2022
Risankizumab effective against refractory psoriatic arthritis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

