https://doi.org/10.55788/a77a6ab5
TAILOR-PCI, presented by Prof. Naveen Pereira (Mayo Clinic, USA), is the largest trial to date to investigate the clinical utility of using genetic testing to detect the clopidogrel loss-of-function (LOF) genotype to guide antiplatelet therapy in patients undergoing percutaneous coronary intervention (PCI). The trial enrolled 5,302 patients who had had PCI with stenting. Patients received standard antiplatelet therapy with clopidogrel 75 mg/day without genetic testing or antiplatelet therapy prospectively guided by genotyping for the clopidogrel reduced-function CYP2C19 alleles. Of the tested patients, 35% was found to have the clopidogrel LOF variant. They received ticagrelor 90 mg daily, whereas patients without the LOF variant were treated with clopidogrel. The primary composite endpoint consisted of CV death, myocardial infarction, stroke, definite or probable stent thrombosis, and severe recurrent ischaemia.
After 1 year, 4% of patients receiving genetically guided treatment experienced a primary endpoint event versus 5.9% of patients who were treated conventionally (adjusted HR 0.66; 95% CI 0.43- 1.02; P=0.56), showing a neutral result for the primary endpoint. An exploratory analysis indicated that there was a lower rate of 40% associated with those who were genotyped (HR 0.60; 95% CI 0.41-0.89; P=0.011). Interestingly, the rate of adverse events was significantly reduced by 79% in the first 3 months of treatment among patients who received genetically-guided therapy compared with those who did not. Prof. Pereira pointed out that, as the risk of adverse events is highest immediately after PCI, the potential benefit of genetically-guided therapy has the largest impact in this particular period. The study might have been underpowered as a result of recent improvements in care, such as the use of drug-coated stents, which may have reduced the expected rates of adverse events. Further studies are planned, including a cost-effectiveness analysis of genetically-guided therapy based on long-term follow-up of these patients.
- Pereira NL, et al. Abstract 402-12. ACC/WCC 28-30 March 2020.
Posted on
Previous Article
« Edoxaban: alternative to warfarin after surgical aortic or mitral valve procedures? Next Article
Subgroup analysis VOYAGER PAD »
« Edoxaban: alternative to warfarin after surgical aortic or mitral valve procedures? Next Article
Subgroup analysis VOYAGER PAD »
Table of Contents: ACC/WCC 2020
Featured articles
Heart Failure and Cardiomyopathies
Mavacamten shows promising results in non-obstructive hypertrophic cardiomyopathy
Vericiguat shows beneficial effects in a very high-risk HF population
No role for sodium nitrite in out-of-hospital cardiac arrest
Vascular Medicine and Thromboembolism
Rivaroxaban and aspirin effective and safe for PAD patients
TAILOR-PCI misses endpoint but still provides valuable insights
Edoxaban: alternative to warfarin after surgical aortic or mitral valve procedures?
Bleeding reduction post-TAVI with OAC alone vs OAC + clopidogrel
Apixaban offers new perspective for cancer patients in need of anticoagulation
Rivaroxaban superior to enoxaparin in preventing VTE in non-major orthopaedic surgery
Interventional Cardiology
TAVR safe and effective in low-risk bicuspid aortic stenosis patients
TAVR model reveals differences in hospital outcomes
2-year results show non-significant outcomes TAVR vs surgery in severe aortic stenosis
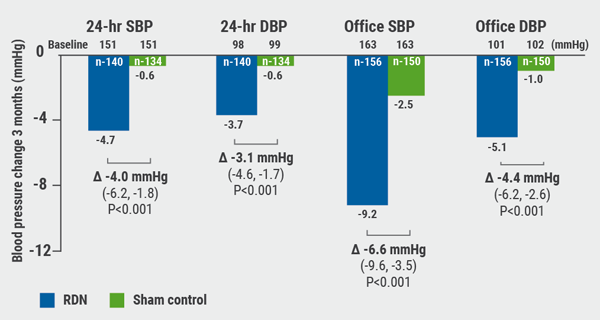
Renal denervation better than sham for blood pressure
Infusion of ethanol in the vein of Marshall for persistent AF
Atrial Fibrillation/Acute Coronary Syndrome
Fewer adverse events with ticagrelor monotherapy after 3 months DAPT
TWILIGHT sub-study: same outcomes for diabetes patients
TWILIGHT sub-study: complex PCI patients
LAAO Watchman registry data positive
Apixaban in AF patients with recent ACS/PCI: Drop aspirin after 30 days
Genetics and Prevention
Homozygous FH responds to alirocumab
Evinacumab significantly reduces LDL-C in homozygous FH patients
Higher serum levels of eicosapentaenoic acid correlate with reduced CV events
Quit smoking: vaping + counselling helps
Related Articles
September 8, 2020
Renal denervation better than sham for blood pressure
September 8, 2020
TAVR versus surgery in older patients
September 8, 2020
TWILIGHT sub-study: same outcomes for diabetes patients
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

