Both the European and US guidelines for the management of lupus nephritis (LN) are almost 9 years old [1,2]. They propose mycophenolate mofetil (MMF) or cyclophosphamide as first-line agents with the addition of glucocorticoids for optimal responses. Second-line agents include rituximab or calcineurin inhibitors. Naturally, these current guidelines are mainly based on clinical evidence and do not account for new perceptions of pathology and the latest studies.
Therefore, Prof. Joan T. Merrill (Oklahoma Medical Research Foundation, USA) covered the new therapies in the drug pipeline in 2020 for LN [3]. The first candidate is the anti-CD20 monoclonal antibody obinutuzumab that was evaluated as add-on treatment to MMF versus placebo plus MMF in a phase 2 trial. To get a better understanding of the efficacy of obinutuzumab, corticosteroids were rapidly tapered. The overall response rates in the obinutuzumab group reached 55.6%, statistically significantly superior to the placebo group (35.5%; P=0.0246). Adverse events were similar among the groups.
Another interesting agent is the B-cell activating factor (BAFF) inhibitor belimumab. In a phase 3 trial, belimumab was added to standard-of-care. This led to a significantly higher chance of achieving a partial and complete response, which was maintained through week 104 compared with placebo (P=0.002 for both comparisons).
Another interesting agent is the calcineurin inhibitor voclosporin, which has an improved safety profile compared with other calcineurin inhibitors. This small modification results in less pharmacokinetic and pharmacodynamic variability. The substance was created by making a small structural change to cyclosporine. Previously, voclosporin was assessed within the AURA phase 2b trial which included 265 patients, all of whom were on a baseline medication of MMF and steroids. In AURA, 32.6% of patients on twice daily (BID) 23.7 mg of voclosporin achieved complete remission as well as 27.3% on 39.5 mg BID versus 19.3% on placebo. This trial also tapered steroids fast to better recognise the treatment effect of voclosporin. Unfortunately, safety data raised some concerns, because the dosing group treated with 23.7 mg BID had far more serious adverse events.
This year, a phase 3 voclosporin trial met its primary endpoint of renal response at week 52: this was seen in 40.8% of patients receiving voclosporin (23.7 mg BID) plus MMF (1 g BID) and a rapid steroid taper compared with 22.5% of those given MMF and tapered steroids alone (P<0.001) [4]. In this trial, the safety profile was similar in the 2 arms, with serious adverse events being reported in 20.8% of the voclosporin group and 21.3% of the control group. Serious infections were seen in 10.1% of the voclosporin group and 11.2% of controls. Hence, the future looks brighter for the management of LN.
- Bertsias GK, et al. Ann Rheum Dis 2012:71:1771-82.
- Hahn BH, et al. Arthritis Care Res 2012;64:797-808.
- Merrill JT, et al. New therapies for LN in 2020. 4S060, ACR Convergence 2020, 5-9 Nov.
- Arriens C, et al. Abstract OP0277, EULAR 2020 eCongress, 3-6 June.
Posted on
Previous Article
« Signs of benefit for T2T in axial spondyloarthritis Next Article
Lupus nephritis biomarkers: moving toward an omic-driven approach »
« Signs of benefit for T2T in axial spondyloarthritis Next Article
Lupus nephritis biomarkers: moving toward an omic-driven approach »
Table of Contents: ACR 2020
Featured articles
Late-Breaking News
Gout treatment with febuxostat: no higher cardiovascular mortality
New agent with great potential for the treatment of giant cell arteritis in the pipeline
Autotaxin inhibitor successful in the first trial in diffuse cutaneous systemic sclerosis
JAK inhibition as a treatment option for ankylosing spondylitis
Spotlight on Rheumatoid Arthritis
Persuasive long-term results for JAK inhibition in rheumatoid arthritis
Rheumatoid arthritis: new EULAR treatment guidelines
Rheumatoid arthritis and interstitial lung disease: a deadly combination
COVID-19 – What Rheumatologists Need to Know
COVID-19 in patients with rheumatic disease: most report mild disease
Poor disease control: a risk factor for severe COVID-19
No heightened outcome risk for rheumatic patients with COVID-19
What Is Hot in Lupus Nephritis?
Lupus nephritis biomarkers: moving toward an omic-driven approach
Lupus nephritis: new therapies on the horizon in 2020
Spondyloarthritis – The Beat Goes On
Artificial intelligence can help in the diagnosis of axSPA
Resolution of dactylitis or enthesitis is associated with improvements in joint and skin symptoms
Promising novel treatment option for psoriatic arthritis
How to Diagnose Large Vessel Vasculitis: Promises and Pitfalls
How to choose imaging modalities in large vessel vasculitis
Diagnosis of large vessel vasculitis with imaging
Osteoarthritis – Novel Developments
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate
Anticoagulation with vitamin K antagonist is associated with risk of knee and hip replacement
Osteoporosis – New Data
Bisphosphonate use: Asian American women have a smaller treatment benefit
Inflammatory disease as a risk factor for fractures
Best of the Posters
No progression of osteoarthritis with corticosteroid injections
Hydroxychloroquine use: no indication for arrhythmias in RA and SLE patients
Children with rheumatic disease have no greater risk of a COVID-19 infection
Insufficient antimalarial supply for rheumatic disease treatment in the early COVID-19 pandemic
Related Articles
September 4, 2019
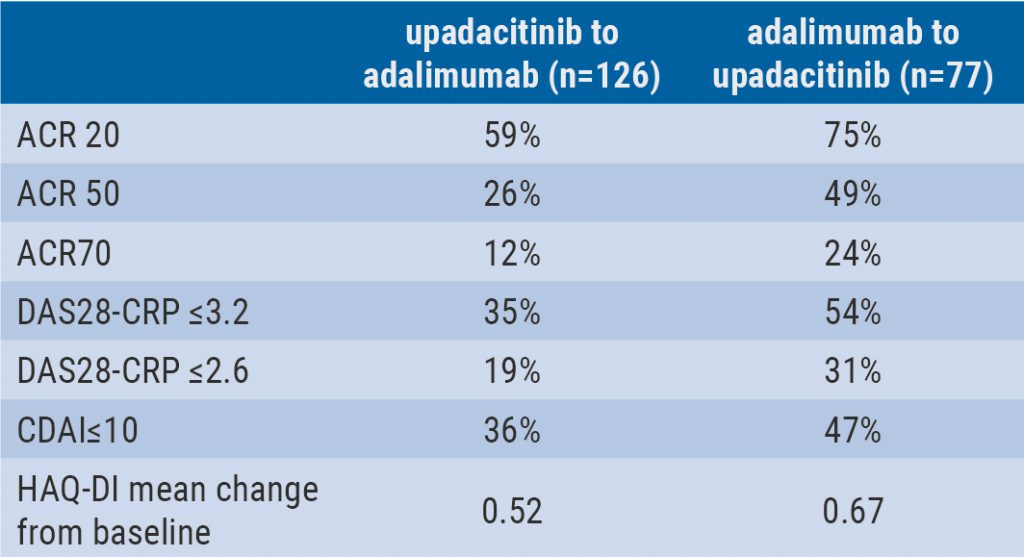
Switching upadacitinib and adalimumab is beneficial in refractory RA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

