“Our registry is a global initiative where cases from Europe are entered by the EULAR and cases in the USA by the ACR,” Prof. Rebecca Grainger (University of Otago, New Zealand) explained [1].
Three analyses were presented during the meeting. The risk of hospitalisation was assessed after the first month of the registry in the European and US cohort, risk factors for death in July in the American cohort, and outcome disparities in the global cohort that included data until August. In the first analysis, 600 cases were included: 277 were hospitalised (46%), 55 died (9%). Most patients suffered from rheumatoid arthritis (RA; 38%) and comorbidities were common. Patients aged >65 years had a 2.55-fold increased risk of hospitalisation. The hospitalisation risk of patients that were treated with a prednisone-equivalent of over 10 mg/day was 2.1-fold elevated. Comorbidity of different organ systems was associated with an up to 3-fold elevated risk of hospitalisation. “It is worth noting that the pre-COVID-19 use of DMARDs or biologics was associated with a reduced risk of hospitalisation,” Prof Grainger said.
In the second analysis, risk factors for death due to a SARS-CoV-2 infection were analysed in 1,324 US cases. In this analysis, Black, Asian American, and Latinx patients had a higher risk of hospitalisation, whereas there was no difference in mortality. Latinx patients had a more than 3-fold elevated risk for ventilatory support.
In the largest analysis, a total of 3,729 patients (two-third from Europe and one-third from the USA) were included. The risk of death from COVID-19 was associated with age, male gender, ever smokers, but the latter only in RA patients, and moderate-to-severe disease activity. COVID-19 fatalities were associated with no DMARD use, both sulfasalazine and rituximab treatment, and therapy with glucocorticoids >10 mg per day. As Prof. Grainger explained, these data reveal some learning points (see Figure). “First, it is important to control disease activity as reduced odds of hospitalisation were seen in patients treated with biologic and targeted systemic DMARDs in analysis 1 and there were higher odds of death in patients with moderate-to-high disease activity in analysis 3,” Prof. Grainer said. Second, therapy with glucocorticoids should be minimised and possibly be <10 mg/day, as higher doses are associated with an increased risk for hospitalisation and death. Due to worse outcome in ethnic minority groups, one should advocate measures to protect these people.
Figure: 5 learning points from International COVID-19 Registries [1]
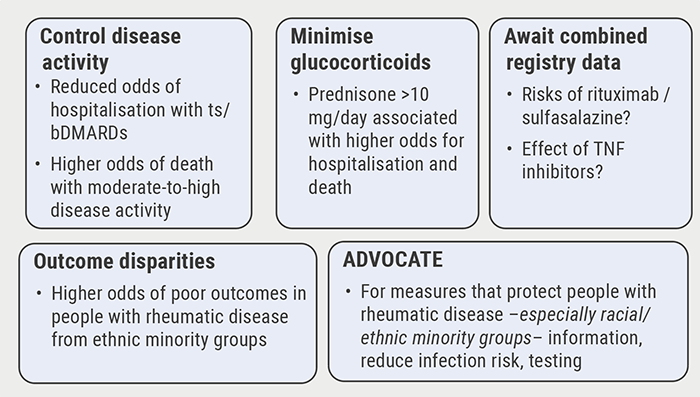
ts, targeted systemic; b, biologic.
- Grainger R, Lessons from the COVID-19 Global Rheumatology Registry: Epidemiology, Risk Factors & Outcomes. ACR Convergence 2020, 5-9 Nov.
Posted on
Previous Article
« No heightened outcome risk for rheumatic patients with COVID-19 Next Article
COVID-19 in patients with rheumatic disease: most report mild disease »
« No heightened outcome risk for rheumatic patients with COVID-19 Next Article
COVID-19 in patients with rheumatic disease: most report mild disease »
Table of Contents: ACR 2020
Featured articles
Late-Breaking News
Gout treatment with febuxostat: no higher cardiovascular mortality
New agent with great potential for the treatment of giant cell arteritis in the pipeline
Autotaxin inhibitor successful in the first trial in diffuse cutaneous systemic sclerosis
JAK inhibition as a treatment option for ankylosing spondylitis
Spotlight on Rheumatoid Arthritis
Persuasive long-term results for JAK inhibition in rheumatoid arthritis
Rheumatoid arthritis: new EULAR treatment guidelines
Rheumatoid arthritis and interstitial lung disease: a deadly combination
COVID-19 – What Rheumatologists Need to Know
COVID-19 in patients with rheumatic disease: most report mild disease
Poor disease control: a risk factor for severe COVID-19
No heightened outcome risk for rheumatic patients with COVID-19
What Is Hot in Lupus Nephritis?
Lupus nephritis biomarkers: moving toward an omic-driven approach
Lupus nephritis: new therapies on the horizon in 2020
Spondyloarthritis – The Beat Goes On
Artificial intelligence can help in the diagnosis of axSPA
Resolution of dactylitis or enthesitis is associated with improvements in joint and skin symptoms
Promising novel treatment option for psoriatic arthritis
How to Diagnose Large Vessel Vasculitis: Promises and Pitfalls
How to choose imaging modalities in large vessel vasculitis
Diagnosis of large vessel vasculitis with imaging
Osteoarthritis – Novel Developments
Knee osteoarthritis patients with indicators of inflammation could profit from methotrexate
Anticoagulation with vitamin K antagonist is associated with risk of knee and hip replacement
Osteoporosis – New Data
Bisphosphonate use: Asian American women have a smaller treatment benefit
Inflammatory disease as a risk factor for fractures
Best of the Posters
No progression of osteoarthritis with corticosteroid injections
Hydroxychloroquine use: no indication for arrhythmias in RA and SLE patients
Children with rheumatic disease have no greater risk of a COVID-19 infection
Insufficient antimalarial supply for rheumatic disease treatment in the early COVID-19 pandemic
Related Articles
August 14, 2020
New nanoparticle promising future agent in RA
May 17, 2022
JAK inhibitors: A risk assessment
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

