“ILD can be considered as a large group of rare to ultra-rare molecular lung diseases. Over 150 diagnoses can be categorised in this group, and the underlying causes are mostly unknown,” he explained, before giving an overview of the ILD classification scheme. Categorised in a separate box linked to RA, polymyositis/dermatomyositis, scleroderma, and Sjögren’s syndrome, was CTD; although Dr Grutters pointed out that CTD and ILD seen in these patients show a pattern of interstitial pneumonitis (IP). “This is CTD-IP, because RA patients can show all kinds of diffuse ILD due to other causes,” he said. Evaluating different CTDs will reveal different histological and high-resolution computed tomography (HRCT) patterns. RA patients frequently present the usual IP pattern which is similar to what is seen in idiopathic pulmonary fibrosis (IPF).
The diagnosis of CTD and ILD starts with a suspicious ILD; other causes of lung disease and/or abnormalities must be excluded. The diagnostic process starts with a basic medical and physical examination, taking a medical history, routine lab test, X-rays, and lung function screening test. Dr Grutters emphasised the importance of taking a complete patient history of environmental exposures at home and at work, as well as prior drug use (nitrofurantoin). Other tests include myositis testing, use of specific antibodies, and HRCT, “which is by far the most central because it reveals the typical features of fibrosis; the IP pattern can be well-differentiated and the extent of disease can be assessed. It may also show co-morbidities like pulmonary hypertension,” he added. Dr Grutters and his team frequently use bronchoalveolar lavage (BAL) which is an important tool for supporting diagnoses related to specific findings; it may exclude infections, asbestos, and alveolar proteinosis. As part of the diagnostic process, Dr Grutters mentioned the importance of multidisciplinary discussion in IPF diagnosis; it leads to consensus diagnoses, improves the accuracy, and it may avoid unnecessary testing.
Current treatment options are immunosuppressive drugs such as cyclophosphamide, azathioprine, mycophenolate, methotrexate, or rituximab, with mycophenolate emerging as the leading treatment [1-3]. However, there is not much evidence for ILD treatment; most comes from randomised controlled trials in scleroderma. Steroids are important for acute and fulminant manifestations of idiopathic inflammatory myositis syndrome. Besides medication, one-third of all RA-ILD worldwide receive lung transplantation with survival benefits in patients with systemic disease and end-stage fibrosis versus IPF.
Novel treatment options are being investigated, as the understanding of systemic sclerosis and associated ILD has improved in recent years. Targeted therapy against IL-6 is an appealing strategy, but trials of tocilizumab, abatacept, and riociguat have been unsuccessful. However, tocilizumab preserved lung function in patients with early systemic sclerosis, so will be investigated further.
New in the field is anti-fibrotic therapy with pirfenidone and nintedanib. “Results of the SENSCIS trial have been presented recently at the American Thoracic Society (ATS) conference in Dallas, USA. Patients with systemic sclerosis-associated ILD (n=576) who had more than 10% fibrosis on HRCT were studied. Half of them were mycophenolate users. Patients were randomised 1:1 to receive 150 mg of nintedanib vs placebo. The results showed that nintedanib had a benefit in reducing the rate of forced vital capacity (FVC) decline, compared with placebo (the annual rate of change in FVC was -52 mL per year in the nintedanib group and -93 mL per year in the placebo group). There were significant side effects, especially diarrhoea, which was also observed in the initial INPULSIS-1 and -2 trials [4].
“Anti-fibrotic treatment will become a game-changer. We must figure out which patients are best treated with what drug. There usually is a combination of inflammation and fibrosis, so anti-inflammatory or anti-fibrotic treatment first?” To decide treatment approach, multidisciplinary discussion is vital: considering individual patient data, assessing the features and extent of inflammation, and progressiveness of fibrosis. “It is an interesting time because of the multiple studies being conducted in ILD/CTD. We have to await the data of current and future trials on rituximab, cyclophosphamide, pirfenidone, and tocilizumab” concluded Dr Grutters. Existing RA literature in ILD supports the idea that rituximab therapy is also beneficial at halting progression.
- Tashkin DP, et al. N Engl J Med. 2006 Jun 22;354(25):2655-66.
- Wiertz IA, et al. Eur Respir J. 2018 Apr 19;51(4).
- Ueda T, et al. Respir Investig. 2018 Jan;56(1):14-20.
- Richeldi L, et al. N Engl J Med. 2014 May29;370(22):2071-82.
Posted on
Previous Article
« What is new in osteoarthritis Next Article
Inflammation may change the course of Parkinson’s disease »
« What is new in osteoarthritis Next Article
Inflammation may change the course of Parkinson’s disease »
Table of Contents: EULAR 2019
Featured articles
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA
Rheumatoid Arthritis
Cohort study shows improvement during 25 years of RA treatment
Filgotinib in RA patients with inadequate response or naïve to methotrexate
Clinical effectiveness of fenebrutinib in RA patients with methotrexate or TNFi failure
Short methotrexate stop is safe in patients with RA
Tofacitinib is safe according to real-world data analysis
Tapering of prednisone in RA patients who achieved low disease activity or remission with tocilizumab
Efficacy and safety of E6011 in RA patients with inadequate response to methotrexate
Preliminary efficacy and safety data of RG6125 in RA patients with an inadequate response to TNF inhibitors
Integrated 10-year analysis confirms safety profile abatacept
Switching among multiple infliximab biosimilars does not cause immunogenicity
Switch to sarilumab from adalimumab is efficacious and safe
Axial Spondyloarthritis
Treat-to-target approach emerging in axial spondyloarthritis
NSAIDs consumption is linked to patient-assessed disease activity and decreases with use of TNF inhibitors
Psoriatic Arthritis
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA
Efficacy and safety of bimekizumab in patients with active PsA
Filgotinib is efficacious and safe in PsA
Ixekizumab improves signs and symptoms in TNFi-naïve PsA patients
Etanercept and methotrexate as first-line treatment in PsA
Unacceptable pain is common in patients with psoriatic arthritis
Osteoarthritis and Osteoporosis
Miscellaneous
Interstitial lung disease in rheumatic diseases and systemic sclerosis
Emapalumab in patients with macrophage activation syndrome
Support for tocilizumab use in giant cell arteritis
Related Articles
September 4, 2019
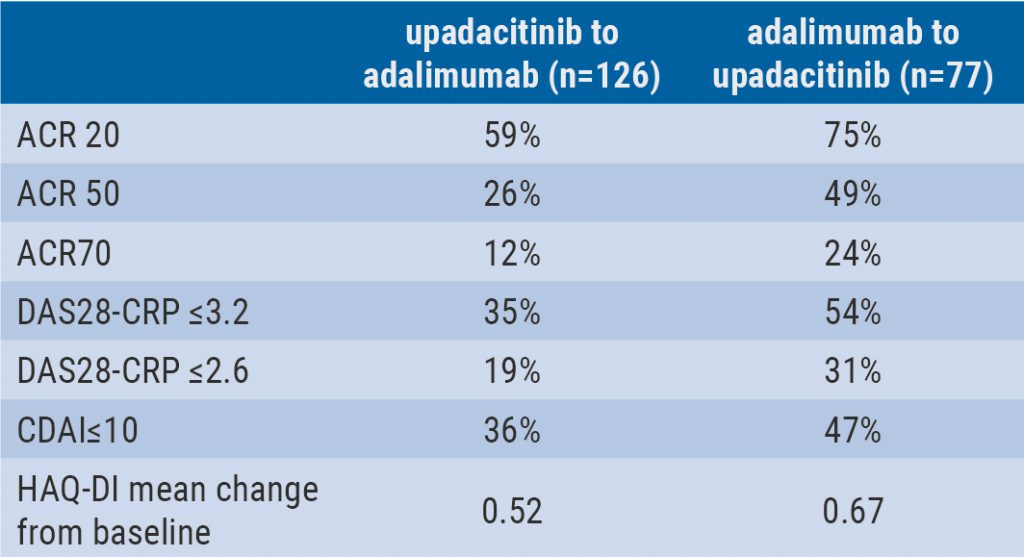
Switching upadacitinib and adalimumab is beneficial in refractory RA
September 4, 2019
Short methotrexate stop is safe in patients with RA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

