This study was conducted by Dr Tor Olofsson (Lund University, Sweden) et al. “It is time to shift gears. We will focus on observational studies and old medications instead of randomised controlled trials and new drugs, and we are looking at pain specifically,” said Dr Olofsson. “A swift background; when asked to prioritise between different domains in which patients are most keen on seeing an improvement, in many studies, pain has turned out as the number one. Furthermore, the prevalence of concurrent fibromyalgia is ≥30% in PsA patients compared with about 2% in the general population [2]. Recently, there is also a growing awareness of an uncoupling between pain and inflammation. However, studies of remaining pain have so far mainly been conducted in rheumatoid arthritis. Therefore, we aimed to assess unacceptable pain, despite inflammation being controlled during the year after starting a first TNF inhibitor (TNFi) therapy in PsA patients” said Dr Olofsson.
PsA patients starting a first TNFi treatment (n=352) between 2004 and 2010 were identified in the prospective, observational South Swedish Arthritis Group register. About half of them were women (48%), the mean age was 47 years old, and mean disease duration 10 years. At the onset of TNFi therapy, 63% of patients had ongoing methotrexate and 68% were on any conventional disease-modifying-anti-rheumatic drugs (DMARDs). Unacceptable pain was defined as >40 mm on a VAS of pain (scale 0-100 mm), based on the patient acceptable symptom state (PASS), and concomitant inflammation control was captured through C-reactive protein (CRP) <10 mg/L in combination with <1 swollen joint count. Assessments were performed at baseline, and 1.5, 3, 6, and 12 months after starting TNFi therapy. Analyses were further conducted in relation to EULAR treatment response, after 3 months (good, moderate, no response). Differences in pain measures between treatment response groups were predicted by regression analysis.
At the start of TNFi therapy, 85% of patients reported unacceptable pain, which declined to 43% after 3 months and then remained stable, reaching 39% at 12 months. The proportion of patients who had unacceptable pain despite inflammation control was largely unchanged over the study period (24% at treatment start, 27% at 3 months, and 26% at 12 months). Unacceptable pain at 3 months was strongly related to EULAR 3-month response (24% of good responders vs 79% of nonresponders; P<0.001). This relationship was less pronounced among patients with unacceptable pain despite inflammation control (19% of good responders vers.us 37% of nonresponders; P=0.016). Among EULAR good responders, unacceptable pain irrespective of inflammation control constituted 81% of all unacceptable pain at 3 months. These findings need to be tempered by factors including the fact that the CRP and other inflammatory markers may be normal in PsA and factors such as polyenthesitis that is difficult to recognise and also not associated with elevated inflammatory markers.
- Roseman C, et al. Abstract OP0112. EULAR 2019.
- Häuser W, Fitzcharles MA. Dialogues Clin Neurosci. 2018 Mar;20(1):53-62.
Posted on
Previous Article
« NSAIDs consumption is linked to patient-assessed disease activity and decreases with use of TNF inhibitors Next Article
Etanercept and methotrexate as first-line treatment in PsA »
« NSAIDs consumption is linked to patient-assessed disease activity and decreases with use of TNF inhibitors Next Article
Etanercept and methotrexate as first-line treatment in PsA »
Table of Contents: EULAR 2019
Featured articles
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA
Rheumatoid Arthritis
Cohort study shows improvement during 25 years of RA treatment
Filgotinib in RA patients with inadequate response or naïve to methotrexate
Clinical effectiveness of fenebrutinib in RA patients with methotrexate or TNFi failure
Short methotrexate stop is safe in patients with RA
Tofacitinib is safe according to real-world data analysis
Tapering of prednisone in RA patients who achieved low disease activity or remission with tocilizumab
Efficacy and safety of E6011 in RA patients with inadequate response to methotrexate
Preliminary efficacy and safety data of RG6125 in RA patients with an inadequate response to TNF inhibitors
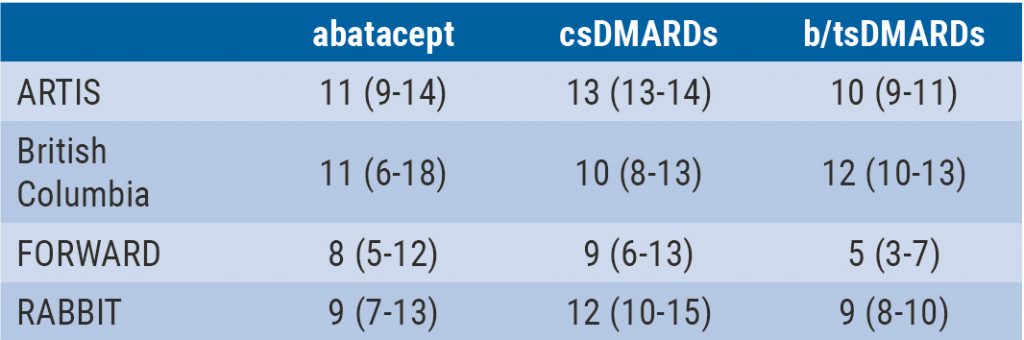
Integrated 10-year analysis confirms safety profile abatacept
Switching among multiple infliximab biosimilars does not cause immunogenicity
Switch to sarilumab from adalimumab is efficacious and safe
Axial Spondyloarthritis
Treat-to-target approach emerging in axial spondyloarthritis
NSAIDs consumption is linked to patient-assessed disease activity and decreases with use of TNF inhibitors
Psoriatic Arthritis
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA
Efficacy and safety of bimekizumab in patients with active PsA
Filgotinib is efficacious and safe in PsA
Ixekizumab improves signs and symptoms in TNFi-naïve PsA patients
Etanercept and methotrexate as first-line treatment in PsA
Unacceptable pain is common in patients with psoriatic arthritis
Osteoarthritis and Osteoporosis
Miscellaneous
Interstitial lung disease in rheumatic diseases and systemic sclerosis
Emapalumab in patients with macrophage activation syndrome
Support for tocilizumab use in giant cell arteritis
Related Articles
September 4, 2019
Tofacitinib is safe according to real-world data analysis
September 4, 2019
Integrated 10-year analysis confirms safety profile abatacept
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

