Therapeutic options for psoriasis include biologic drugs such as tumour necrosis factor inhibitors (TNFi) and IL-12/23 inhibitors. Bimekizumab is a monoclonal antibody that selectively neutralises both, IL-17 homo-, and heterodimers,” said Dr Ritchlin. “The rationale for blocking both IL-17A and IL-17F is the recent discovery that both contribute to the development of PsA. IL-17A and IL-17F are different isoforms of IL-17 having structural homology and overlapping biological functions. Both are expressed in sites of inflammation and independently cooperate with other cytokines. The study objective was to assess the dose-response, long-term efficacy, and safety of bimekizumab over 48 weeks in patients with active PsA.
The randomised, double- and dose-blind, placebo-controlled, BE ACTIVE phase 2B trial included adult PsA patients (n=206), who had both ≥3 tender and ≥3 swollen joints and a CASPAR score ≥3. Patients were randomised (1:1:1:1:1) to receive subcutaneous bimekizumab 16 mg, 160 mg, 160 mg with 320 mg loading dose, 320 mg, or placebo every 4 weeks, for a double-blind period of 12 weeks. After week 12, patients receiving placebo or bimekizumab 16 mg were re-randomised (1:1) to receive bimekizumab 160 mg or 320 mg for the remaining 36 weeks. All other patients continued on their initial dose (dose-blind period). The primary endpoint was the occurrence of disease worsening, defined by the disease-specific composite measures, including ACR criteria or PASI scores, or clinically significant worsening leading to a major change in treatment.
At baseline, the patients had an average tender joint count of 21.7, an average swollen joint count of 11.5, and 66.5% had a psoriasis body surface area of ≥3% or above. The dropout rate for the study was 8%.
The results showed that at week 12, significantly more patients receiving bimekizumab had achieved an ACR50 response, with rates of 26.8% at the 16 mg dose, 41.5% at the 160 mg dose, and 46.3% at the 160 mg dose + 320 mg loading dose, compared with 7.1% in the placebo group. The 24.4% ACR50 response rate in patients taking the 320 mg dose was not significantly different from placebo. “This may be due in part to this group having more active skin and joint disease than the other groups,” said Dr Ritchlin. By week 48, ACR50 response rates in the 320 mg dose group, including those re-allocated at 12 weeks, had improved in line with those of the other groups. PASI100 response rates among patients receiving bimekizumab ranged from 17.2% to 50.0% at week 12 vs 7.1% in those receiving placebo. These rates continued to increase, reaching up to 61% to 73% at week 48. The safety profile of bimekizumab was consistent with previous reports, with no apparent relationship between dose and treatment-emergent adverse events.
- Ritchlin C. T. , et al. Abstract OP0108. EULAR 2019
Posted on
Previous Article
« Filgotinib is efficacious and safe in PsA Next Article
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA »
« Filgotinib is efficacious and safe in PsA Next Article
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA »
Table of Contents: EULAR 2019
Featured articles
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA
Rheumatoid Arthritis
Cohort study shows improvement during 25 years of RA treatment
Filgotinib in RA patients with inadequate response or naïve to methotrexate
Clinical effectiveness of fenebrutinib in RA patients with methotrexate or TNFi failure
Short methotrexate stop is safe in patients with RA
Tofacitinib is safe according to real-world data analysis
Tapering of prednisone in RA patients who achieved low disease activity or remission with tocilizumab
Efficacy and safety of E6011 in RA patients with inadequate response to methotrexate
Preliminary efficacy and safety data of RG6125 in RA patients with an inadequate response to TNF inhibitors
Integrated 10-year analysis confirms safety profile abatacept
Switching among multiple infliximab biosimilars does not cause immunogenicity
Switch to sarilumab from adalimumab is efficacious and safe
Axial Spondyloarthritis
Treat-to-target approach emerging in axial spondyloarthritis
NSAIDs consumption is linked to patient-assessed disease activity and decreases with use of TNF inhibitors
Psoriatic Arthritis
Efficacy and safety of ixekizumab versus adalimumab in patients with PsA
Efficacy and safety of bimekizumab in patients with active PsA
Filgotinib is efficacious and safe in PsA
Ixekizumab improves signs and symptoms in TNFi-naïve PsA patients
Etanercept and methotrexate as first-line treatment in PsA
Unacceptable pain is common in patients with psoriatic arthritis
Osteoarthritis and Osteoporosis
Miscellaneous
Interstitial lung disease in rheumatic diseases and systemic sclerosis
Emapalumab in patients with macrophage activation syndrome
Support for tocilizumab use in giant cell arteritis
Related Articles

September 4, 2019
Ixekizumab improves signs and symptoms in TNFi-naïve PsA patients
September 4, 2019
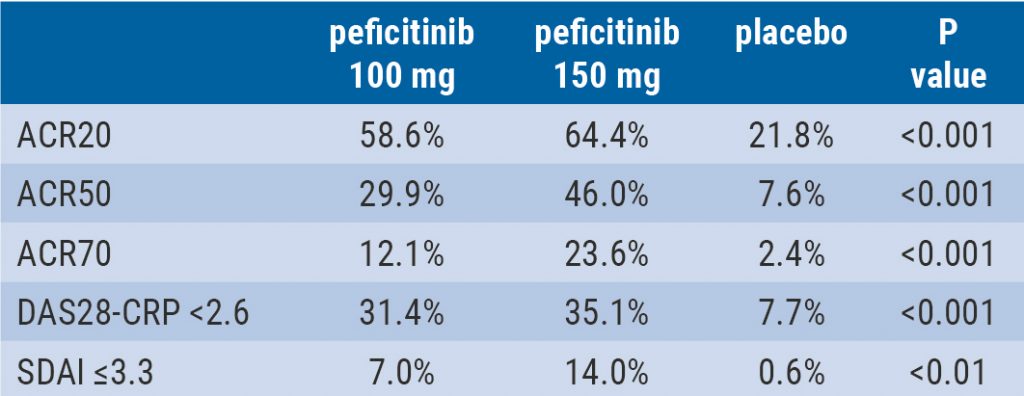
Peficitinib likely efficacious and safe
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

