Every adult produces up to 1.5 litres of saliva per day by the sublingual, the parotid (1/4-1/3, serous), but mainly by the submandibular gland (≥2/3, mucous and serous), according to Prof. Jost. While sialorrhea refers to excessive saliva production, drooling means unintentional loss of saliva from the mouth, he explained.
Common causes of sialorrhea are Parkinson's disease, stroke, amyotrophic lateral sclerosis, traumatic brain injury, or cerebral palsy. Consequences of sialorrhea may be of a social or medical nature. Embarrassment, social isolation, stigmatisation, perioral skin breakdown, pneumonia due to aspiration of saliva, choking, and dehydration, all may lead to increased morbidity and mortality as well as an impaired quality of life.
Multidisciplinary management of sialorrhea consists of speech therapy, which is moderately helpful, functional dysphagia therapy, oral motor training, intra-oral devices, irradiation, oral/transdermal anticholinergics such as atropine or scopolamine, or surgery in therapy-resistant cases. In Europe, 320 μg/ml glycopyrronium is approved for children only. Neither oral drugs nor patches are currently approved by the FDA or EMA for treatment of chronic, troublesome sialorrhea in adults.
However, botulinum neurotoxin type A has been effectively used to reduce saliva production in patients with sialorrhea since 1999 [1]. Many trial data confirmed safety and efficacy of botulinum toxin A and botulinum toxin B formulations in sialorrhea therapy. In the summer of 2018, incobotulinum toxin A has been approved by the FDA for the treatment of patients suffering from sialorrhea. It was the only botulinum toxin preparation in the USA to receive approval for hypersalivation without restrictions on the underlying cause. EMA approval is anxiously awaited. Prof. Jost manages sialorrhea with the help of botulinum toxin injections, and showed pictures of the injection technique for the submandibular gland. While the gland is very superficial in younger patients, longer needles are recommended in older patients. According to Prof. Jost, an ultrasound-guided injection of 100 units incobotulinum toxin A is recommended, distributed in the parotid and submandibular salivary glands.
SIAXI - incobotulinum toxin A effective and safe in sialorrhea
For evaluation of efficacy and safety of incobotulinum toxin A treatment in patients with sialorrhea under more rigorous conditions, Prof. Jost initiated the randomised, multicentre, double-blind, placebo-controlled, pivotal phase 3 study SIAXI with an extension period of dose-blinded active therapy [2]. The study population consisted of 184 adult patients without clinically relevant dysphagia but with chronic troublesome sialorrhea for at least 3 months prior to screening. Hypersalivation was related either to idiopathic, familial, or atypical Parkinson syndromes, stroke, or traumatic brain injury. After salivary glands had been identified, injections were administered using ultrasound guidance in 56.5% of the total study population. Although investigators were encouraged to use ultrasound for guidance of injections, both injections with and without ultrasound guidance (anatomical landmark guidance) were similarly effective as revealed by the results. For treatment, patients received either placebo (n=36) or incobotulinum toxin A (n=74 in both groups), distributed bilaterally in the parotid and submandibular glands in a single injection cycle (16 ± 2 week duration). Two dosages of incobotulinum toxin A (75 units and 100 units) were evaluated. Each treatment consisted of 4 injections into the bilateral parotid and submandibular salivary glands in a 3:2 ratio to avoid worsening of any pre-existing swallowing problems due to salivary thickening.
Prof. Jost presented the clinically meaningful primary efficacy data. The results of the co-primary endpoints of the main study period confirmed efficacy of incobotulinum toxin A. This was demonstrated by improved scores of the Global Impression of Change Scale (GICS) and the reduction of unstimulated salivary flow rate by incobotulinum toxin A (Figure 1). The mROMP drooling scores (modified Radboud Oral Motor inventory for Parkinson's disease subscales), assessing the domains speech, swallowing, and salivary control, improved from study baseline over 16 weeks to a greater extent in patients treated with incobotulinum toxin A compared with placebo. Average mROMP speech and swallowing symptoms scores improved only slightly from study baseline to all post-treatment visits. Incobotulinum toxin A therapy resulted in reduction of saliva production without impairing speech or swallowing abilities, as revealed by the mROMP speech and swallowing symptom scores. No unexpected adverse events of special interest occurred during treatment with incobotulinum toxin A.
These data have led to FDA approval of incobotulinum toxin A 100 units in the US for adults with sialorrhea.
Figure 1: Change from baseline in unstimulated salivary flow rate (uSFR) in the various treatment groups [2]
- Jost WH. Poster 115, TOXINS 2019, Copenhagen, Denmark, 16-19 January.
- Jost WH, et al. Neurology (2019, in press).
Posted on
Previous Article
« Anterocollis posture and deep cervical muscle injections Next Article
Central and peripheral mechanisms in migraine »
« Anterocollis posture and deep cervical muscle injections Next Article
Central and peripheral mechanisms in migraine »
Table of Contents: TOXINS 2019
Featured articles
Pain
Pain subsides before effect on muscles become apparent
Migraine
Central and peripheral mechanisms in migraine
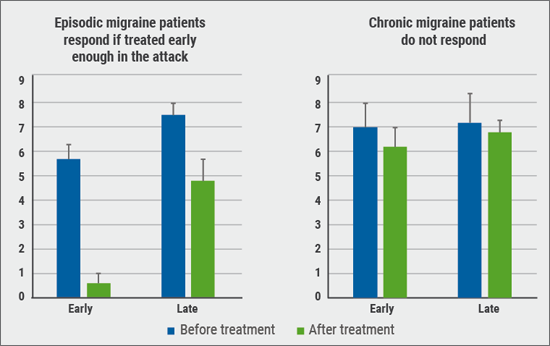
Predictors of response
Spasticity
Why treat spasticity?
ASPIRE: High patient and clinician satisfaction
Cervical Dystonia
Anterocollis posture and deep cervical muscle injections
Daxibotulinum toxin in isolated cervical dystonia
Parkinson
Utility of botulinum toxin in Parkinson’s disease beyond sialorrhea
New Versions of Botulinum Toxins
New Versions of Botulinum Toxins
Related Articles
March 15, 2019
Lessons learned from triptan therapy
March 15, 2019
Why treat spasticity?
March 15, 2019
Diagnosis and treatment
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

