In his keynote lecture, Prof. Stephen McMahon (King’s College London, United Kingdom) talked about two important processes, i.e. peripheral and central sensitisation. He asked, "if you are trying to develop a therapy, where should you be targeting your therapies to alleviate pain? We do not have a very complete answer to that question," he conceded, "but the data that we do have, strongly suggest that peripheral mechanisms are important for many patients." Prof. McMahon concluded that while most patients presumably have a peripheral mechanism driving their chronic pain, the remaining patients may have a central mechanism that dominates. "You might want to stratify those patients to treat them better," he added.
Prof. McMahon presented data relating to neuropathic pain: "It is a small trial, but I think it is indicative of a range of data in the literature. It shows the effect of local anaesthetic block - of lidocaine block - on neuropathic pain behaviour in a smaller group of (mainly diabetic) patients, either with peripheral nerve injury or polyneuropathy. What it shows is that all these patients got a complete, albeit temporary relief of pain by blocking their peripheral nervous system. This is not to say that central pain states are unimportant. I think you can treat chronic pain very effectively with centrally active compounds. We do that with antidepressants, for instance. But the important point is that those central abnormalities seem to be driven in many patients by peripheral abnormalities." Therefore, it is a logical conclusion, he stated, to address peripheral pain in most patients.
Prof. McMahon also talked about the growing interest in neurotoxins, particularly in botulinum toxin A, which may affect nociceptor function in multiple ways, i.e. by receptor trafficking in nociceptor terminals, retrograde transport and cell-to-cell-signalling, trans-ganglionic transport and neurotransmitter release, trans-synaptic transport and block of CNS neurotransmission, and by a direct effect on peripheral non-neuronal cells. Botulinum toxin A has been clinically licensed and tested in many pain states, including migraine, headache, musculoskeletal pain (back pain), trigeminal neuralgia, (peripheral) neuropathic pain, diabetic painful neuropathy, and osteoarthritis. In animal models, botulinum toxin A reversed mechanical hyperalgesia of neuropathic pain (diabetic neuropathy) and inflammatory pain, as in carrageenan (additive in nutrition extracted from red seaweed) inflammation [1], and in human volunteers it has shown to alter pain perception [2]. Increasing evidence for pain reduction derives from case reports and clinical trials, demonstrating efficacy of botulinum toxin when treating patients suffering from neuropathic pain, including post-herpetic neuralgia, post-traumatic and postoperative neuropathies, as well as trigeminal neuralgia.
- Favre-Guilmard C, et al. Eur J Pain. 2017 May;21(5):927-937.
- Paterson K, et al. Ann Neurol. 2014 Apr;75(4):591-6.
Posted on
Previous Article
« Why treat spasticity? Next Article
Diagnosis and treatment »
« Why treat spasticity? Next Article
Diagnosis and treatment »
Table of Contents: TOXINS 2019
Featured articles
Pain
Pain subsides before effect on muscles become apparent
Migraine
Central and peripheral mechanisms in migraine
Predictors of response
Spasticity
Why treat spasticity?
ASPIRE: High patient and clinician satisfaction
Cervical Dystonia
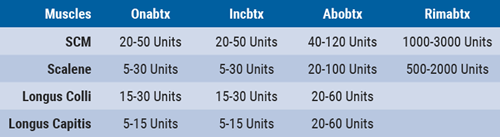
Anterocollis posture and deep cervical muscle injections
Daxibotulinum toxin in isolated cervical dystonia
Parkinson
Utility of botulinum toxin in Parkinson’s disease beyond sialorrhea
New Versions of Botulinum Toxins
New Versions of Botulinum Toxins
Related Articles
March 15, 2019
Predictors of response
March 15, 2019
Diagnosis and treatment
March 15, 2019
Anterocollis posture and deep cervical muscle injections
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

