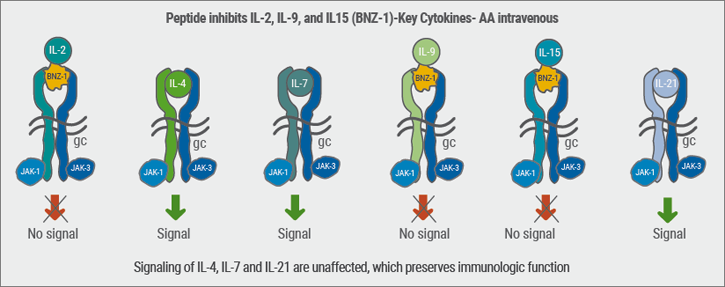
“The problem with this medication, which has the potency of low-to-mid-potency topical corticosteroids is the price: a 60g tube costs 600 US dollars,” said Prof. Simpson. Other topical PDE4 inhibitors are also in development. “JAK inhibitors are definitely entering dermatology, locally and systemically,” said Prof. Simpson. JAKs are key mediators in the signalling pathway of numerous cytokines implicated in the pathogenesis of AD, which include IL-4, -13, and IL-31 (see Figure). [12,13].
Figure: JAK inhibitors influence numerous cells in Atopic Dermatitis. [12,13]

A topical PAN-JAK inhibitor, JTE-052, displayed remarkable efficacy in Japanese patients with moderate-to-severe AD in improving the EASI, the primary endpoint of this trial [14]. Patients were randomised to receive the topical JAK-Inhibitor at 0.25%, 0.5%, 1%, and 3%, as well as the vehicle ointment, or tacrolimus (0.1%); these ointments were applied twice daily for four weeks.
Patients in all JAK-Inhibitor groups experienced a significant change in modified EASI score from baseline, compared with the vehicle group. The improvements appeared to be dose-dependent. “A rapid improvement of pruritus was observed already at Day 1 for the three higher dosing groups,” said Prof Simpson. A
ll adverse events were considered mild or moderate in severity, the majority of them mild; no serious adverse events were reported. It is notable that no clinically significant changes in laboratory parameters or vital signs were reported. Clinical results were similar to tacrolimus ointment 0.1%, but with fewer side-effects and burning. This study suggests that JAK inhibitors in AD are very promising and can provide increased opportunity to tailor treatment to the needs of each individual patient.
The International Eczema Council considered when AD should warrant systemic therapy [15]. “We came to the conclusion that systemic treatment should only be advocated if aggressive topical therapy does not achieve adequate control of the disease,” said Prof. Simpson. A systematic and holistic approach is recommended to assess patients with severe AD and the impact on QoL before systemic therapy.
Steps taken before commencing systemic therapy include considering alternate or concomitant diagnoses (e.g. allergic contact dermatitis), avoiding trigger factors, optimising topical therapy, ensuring adequate patient/caregiver education, treating coexistent infection, assessing QoL, and considering phototherapy. “In many cases, phototherapy is a safe and effective way to enhance topical therapy,” said Prof. Simpson.
10. Simpson, El. oral presentation session F012, AAD Annual Meeting, February 16–20 2018.
11. Ahmed, A. et al. Br J Dermatol 2017 Dec 3.
12. Paller, AS. et al. J Allergy Clin Immunol 2017;140:633–43.
13. Bissonnette, R. et al. Br J Dermatol 2016;175:902–11.
14. Nakagawa, H. et al. P2118, EADV Annual Meeting, September 16–20 2017.
15. Simpson, EL. et al. J AM Acad Dermatol 2017;77:623–33.
Posted on
Previous Article
« Dual JAK/SYK inhibitor and anti-IL-33 blockade Next Article
Restrictive antibiotic use and novel tetracycline »
« Dual JAK/SYK inhibitor and anti-IL-33 blockade Next Article
Restrictive antibiotic use and novel tetracycline »
Table of Contents: AAD 2018
Featured articles
Letter from The Editor
Living in the golden age of psoriasis and atopic dermatitis therapies
Late-breakers
IL-17C inhibition in AD and new oral treatments
Dual JAK/SYK inhibitor and anti-IL-33 blockade
Psoriasis: Selective IL-23 blocker, analysis of VOYAGE-2, dual IL-17 inhibitor and ustekinumab
Hyperhidrosis: Soft molecule and anticholinergic towelettes
Behcet’s syndrome and hidradenitis suppurativa
Psoriasis: an update
Oral therapeutics, supersaturation and excimer laser
Psoriasis management online?
What's hot in atopic dermatitis
AD sleep disturbance, antihistamines and osteoporosis
New topical and systematic treatments
Acne management
Winter effect and preventing scarring
Restrictive antibiotic use and novel tetracycline
Alopecia Areata
Melanoma
Melanoma incidence continues to rise in Europe
Lesions in paediatric patients and possible correlation with coffee drinking
CNNs and targeted combination therapy
Pearls of the posters
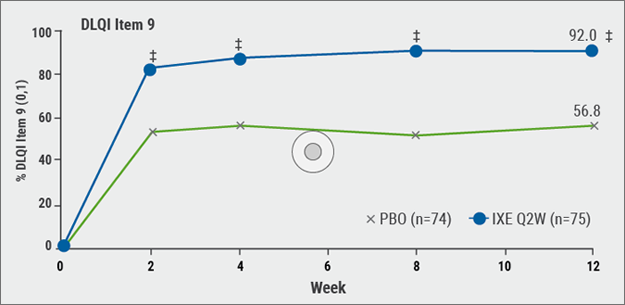
Improvement in impact of genital psoriasis on sexual activity with use of ixekizumab
Intralesional cryosurgery and itching in psoriasis
Related Articles

December 20, 2018
Oral therapeutics, supersaturation and excimer laser
December 20, 2018
New agents and combination therapy
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

