IL-17C Inhibition in AD: a new treatment approach
Last autumn, the first biologic for atopic dermatitis (AD) was approved in Europe. But more is yet to come!
Another interesting approach is blockade of interleukin (IL)-17C, which was shown to be remarkably effective in a randomised controlled, dose-escalation, phase-1 trial presented by Prof. Diamant Thaçi MD, University Clinic Schleswig-Holstein [1]. “In moderate-to-severe AD we have a clear unmet medical need for treatments that are safe and efficacious”, Prof. Thaci emphasised during the presentation of the data.
The rationale for this trial was experimental evidence that IL-17C induces expression of proinflammatory cytokines, mediators and antimicrobial peptides in epithelial cells and is thus closely related to dermal inflammation. This has been shown to be distinct from other members of the IL-17 cytokine family.
In the trial, 25 subjects with moderate-to-severe AD received four weekly infusions with three different doses, and then a 10-week follow-up period. 83% of patients (five out of six) at the highest dose reached at least 50% improvement on the Eczema Area and Severity Index (EASI-50) at Week 4. The onset of activity occurred within two to four weeks, depending on the dose administered.
Pooled data across all three dose cohorts showed a 72% improvement of AD symptoms at Week 12 compared to baseline in patients treated with the IL-17C blocker. Even at Week 4, 58% had already reached EASI-50 response (compared to 32% with the placebo). The agent was well-tolerated with no safety signals detected. All adverse drug reactions observed were mild-to-moderate and transient in nature. It is notable that activity was maintained more than two months after the last treatment.
"Both the first signs of clinical activity and the sustained response, lasting up to two months after treatment discontinuation, support further clinical development of this antibody," concluded Prof. Thaci.
A Phase 2 trial will commence in 2018.
But also new oral treatments on the horizon
The selective Janus kinase (JAK)-1 inhibitor, upadacitinib, is currently being investigated for the treatment of patients with AD and other inflammatory indications. A Phase 2b trial, presented by Prof. Emma Guttmann-Yassky of Mount Sinai Hospital, showed promising results in patients with moderate-to-severe atopic dermatitis [2].
Patients who were inadequately controlled by topical treatment, or for whom topical treatments were not medically advisable, were randomised to once-daily upadacitinib monotherapy 7.5, 15, or 30 mg, or placebo. The primary endpoint of this dose finding study was a mean percentage improvement in EASI score from baseline to Week 16. Janus kinase upadacitinib showed a clear dose-response effect and good differentiation between doses of 7.5, 15 and 30 mg, and placebo. At Week 16, all upadacitinib dose groups experienced statistically significant improvements compared to placebo. Mean EASI scores improved 23% for placebo vs. 74.4% for the 30 mg dose upadacitinib over the 16-week trial.
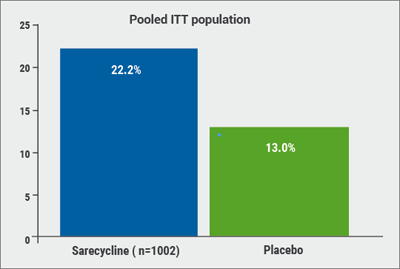
Upadacitinib was also effective in relation to a couple of key secondary endpoints such as EASI 75 or EASI 90 response, or clear or almost-clear skin, according to the investigator´s global assessment (IGA 0/1) (see Figure). “Even the lowest dose gave us good EASI 90 results, while 50% of patients on the highest dose showed EASI 90,” said Prof. Guttman-Yassky. “And we saw no serious adverse events.” The agent displayed a rapid onset of action with significant differences compared to placebo after only two weeks; maximum efficacy was reached after four weeks and maintained until Week 16.
Figure: Upadacitinib was effective in a dose-dependent way regarding EASI response in moderate-to-severe AD. [2]

Upadacitinib successfully lowered pruritus (assessed on a numerical rating scale) compared to placebo. The most common adverse events were upper respiratory tract infections in >10% of patients and exacerbations of AD. No herpes zoster, malignancies, death or cases of pulmonary embolism or deep vein thrombosis were reported. “I think these are quite exciting data”, concluded Prof. Guttman-Yassky.
A 72-week extension of this trial will be reported later this year.
1. Thaci, D. Abstract 6752, AAD Annual Meeting, February 16–20 2018.
2. Guttman, E. Abstract 6533, AAD Annual Meeting, February 16–20 2018.
Posted on
Previous Article
« New agents and combination therapy Next Article
Lesions in paediatric patients and possible correlation with coffee drinking »
« New agents and combination therapy Next Article
Lesions in paediatric patients and possible correlation with coffee drinking »
Table of Contents: AAD 2018
Featured articles
Letter from The Editor
Living in the golden age of psoriasis and atopic dermatitis therapies
Late-breakers
IL-17C inhibition in AD and new oral treatments
Dual JAK/SYK inhibitor and anti-IL-33 blockade
Psoriasis: Selective IL-23 blocker, analysis of VOYAGE-2, dual IL-17 inhibitor and ustekinumab
Hyperhidrosis: Soft molecule and anticholinergic towelettes
Behcet’s syndrome and hidradenitis suppurativa
Psoriasis: an update
Oral therapeutics, supersaturation and excimer laser
Psoriasis management online?
What's hot in atopic dermatitis
AD sleep disturbance, antihistamines and osteoporosis
New topical and systematic treatments
Acne management
Winter effect and preventing scarring
Restrictive antibiotic use and novel tetracycline
Alopecia Areata
Melanoma
Melanoma incidence continues to rise in Europe
Lesions in paediatric patients and possible correlation with coffee drinking
CNNs and targeted combination therapy
Pearls of the posters
Improvement in impact of genital psoriasis on sexual activity with use of ixekizumab
Intralesional cryosurgery and itching in psoriasis
Related Articles
December 20, 2018
Restrictive antibiotic use and novel tetracycline

December 21, 2018
Living in the golden age of psoriasis and atopic dermatitis therapies
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

