https://doi.org/10.55788/7d40a274
The term juvenile idiopathic arthritis subsumes various acquired immune-mediated diseases [1–3]. Currently, treatment options such as conventional synthetic or biologic disease-modifying antirheumatic drugs (csDMARD or bDMARD) are frequently used. “Our patients and parents have been waiting for oral alternatives to injectable drugs and the JAK inhibitors have come at the right time,” Prof. Athimalaipet Ramanan (Bristol Medical School, United Kingdom) expressed as he reported on the phase 3 JUVE-BASIS trial (NCT03773978) [1].
JUVE-BASIS assessed baricitinib in JIA with an unusual design. “All participants, in order to be ethical and to not subject our paediatric patients to placebo, were given access to the drug, and the responders were randomised at 12 weeks on a 1 to 1 basis to either continue the drug or switch to placebo,” Prof. Ramanan explained. The trial included participants with different forms of JIA such as enthesitis-related JIA, polyarticular JIA, and juvenile psoriatic arthritis. The double-blind withdrawal period extended from week 12 through 44 and the primary endpoint was the time to disease flare. Enrolled participants (n=220) had to be between 2 and 18 years old with a history of inadequate response to csDMARD or bDMARD.
At baseline, the mean age of the participants was 13.3 years, and the mean disease duration was 4 years. Of the 220 participants, 52.7% had previously been treated with biologics, 57.7% were on methotrexate, and 32.7% were on corticosteroids.
After the open-label lead-in 12-week period, JIA-ACR30 responses were reached by 76.3%, with corresponding rates for JIA-ACR50 at 63.5%, JIA-ACR70 at 46.1%, and JIA-ACR90 at 20.1%. “But the key was really in the withdrawal phase,” Prof. Ramanan stressed. Of the participants who stayed on baricitinib, 17.1% had a flare compared with 50.6% in the group that was switched to placebo (P<0.001; see Figure). “Not only do those who get switched to placebo have a higher incidence of flaring, but they were also more likely to flare quickly (as quickly as 4 weeks),” Prof. Ramanan commented on this significant result in the primary endpoint with a hazard ratio of 0.241 (P<0.001) in favour of baricitinib.
Figure: Baricitinib significantly increased the time to disease flare and decreased the frequency of disease flares versus placebo [1]
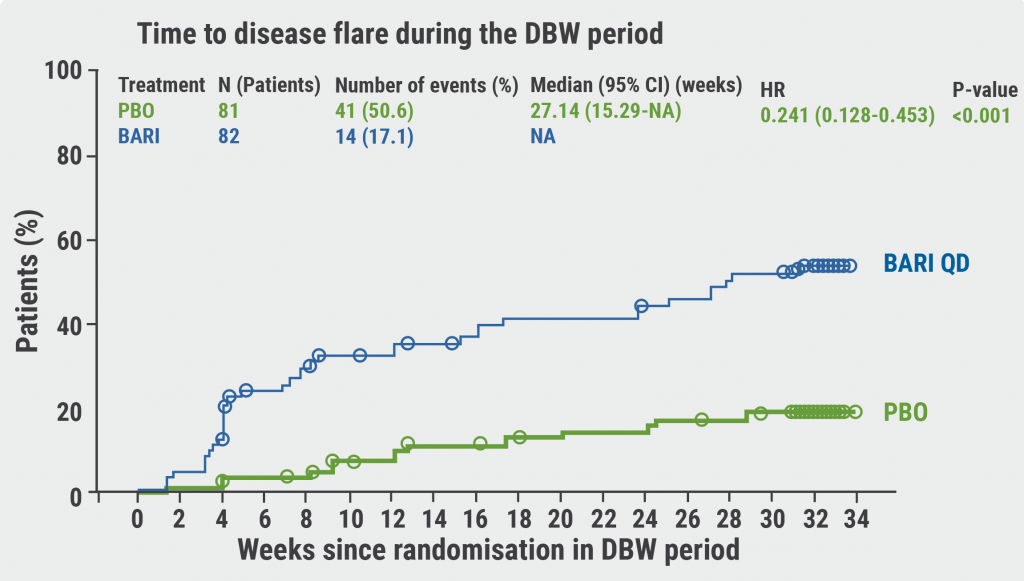
PBO, placebo; BARI, baricitinib; QD, once daily; DBW, double-blind withdrawal; NA, not applicable.
As safety might be even more important in paediatric patients than in adults, adverse events (AEs) were looked at in the lead-in period as well as the double-blind phase. In weeks 0–12, the discontinuation rate due to AEs was 0.9%. During the withdrawal part, 2 participants in the placebo and 1 participant in the baricitinib arm ended the trial because of AEs. From weeks 12–44, treatment-emergent AEs (such as nasopharyngitis, headache, arthralgia, upper respiratory tract infection, and nausea) were observed in 46.9% of placebo and 65.9% of baricitinib participants. Serious AEs (such as COVID-19, gastroenteritis, headache, pulmonary embolism, bronchospasm, suicide attempt, and opportunistic infections) occurred in 3.7% (placebo) and 4.9% (baricitinib) of participants. “These are the short-term safety results, what we in paediatrics are interested in is median and really long-term safety,” Prof. Ramanan added. Overall, the researchers valued the safety results as consistent with the known safety profile of baricitinib.
These results support the oral JAK1/2 agent baricitinib as an alternative treatment for JIA patients with an inadequate response to csDMARD or bDMARD. “These are very interesting findings for our patients and parents of children with JIA,” Prof. Ramanan interpreted the trial results.
- Ramanan AV, et al. Baricitinib in juvenile idiopathic arthritis: a phase 3, double-blind, placebo-controlled, withdrawal, efficacy and safety study. LB0002, EULAR 2022 Congress, 1-4 June, Copenhagen, Denmark.
- Onel KB, et al. Arthritis Rheumatol. 2022;74:553–569.
- Prakken B, et al. Lancet. 2011;377:2138–2149.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Sarilumab for polymyalgia rheumatica led to sustained remission and fewer flares Next Article
Psoriatic arthritis: significant improvement with bimekizumab »
« Sarilumab for polymyalgia rheumatica led to sustained remission and fewer flares Next Article
Psoriatic arthritis: significant improvement with bimekizumab »
Table of Contents: EULAR 2022
Featured articles
Late-Breaking Oral Abstracts
TYK2 inhibition: the future of treating lupus erythematosus?
Psoriatic arthritis: significant improvement with bimekizumab
Baricitinib could open the door to oral treatment for juvenile idiopathic arthritis
Sarilumab for polymyalgia rheumatica led to sustained remission and fewer flares
Spotlight on Rheumatoid Arthritis
Comorbid depression comes with a profoundly higher mortality risk in RA
Preventive treatment with methotrexate benefits pre-RA patients with arthralgia
Risk factors for dementia in RA patients discovered
VTE in global registry data more common in JAK inhibitor-treated RA patients
Spondyloarthropathies – Novel Developments
How to treat enthesitis in 2022
Baseline cardiovascular risk linked to higher rates of MACE in PsA and PsO patients receiving tofacitinib
Treat-to-target dose reduction effective in spondyloarthritis
A novel oral treatment possibility for non-radiographic axSpA on the horizon
Many RA and PsA patients have problems with their sex life
What Is Hot in Osteoarthritis?
New treatments in osteoarthritis
OA associated with alcohol and drug abuse
Body mass index increase associated with structural changes in knee OA
What Is New in Lupus and Scleroderma
Inhibition of Bruton’s tyrosine kinase: a new way of approaching SLE?
Pregnancies in SLE: many complications for mothers and their unborn children
Lupus nephritis: Efficient treatment may reduce the risk of kidney disease advancement
Antifibrotic therapy with nintedanib is beneficial for patients with negative prognostic factors
Best of the Posters
Alarmingly low activity in patients with non-inflammatory and inflammatory rheumatic disease
High prevalence of fibromyalgia in patients with inflammatory bowel disease
Related Articles
May 9, 2019
Topical review
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

