Evidence for BPA
Multiple studies performed in the last six years have shown that BPA improves clinical status and haemodynamics of non-operable CTEPH patients and is associated with a low mortality rate. Based on these findings, Dr Xavier Jaïs (Hôpitaux Universitaires Paris-Sud, France) mentioned that a refined BPA procedure could be considered as a therapeutic approach for this patient population [10-12]. In a French cohort study, which was presented during the ERS meeting, Dr Jaïs and colleagues reported that the outcomes of BPA procedures were better if the surgeons had performed more interventions in the past, providing evidence for a learning curve with respect to the efficacy and safety of this intervention. These and other aspects of BPA are discussed in more detail in a recent review article [13].
BPA-related complications
During the procedure, the main BPA-related complication is vascular injury, which can be associated with or without haemoptysis. The causes of vascular injury include wire perforation, balloon over-dilatation, and high-pressure contrast injection. Signs and symptoms of vascular injury are extravasation of contrast, hypoxaemia, cough, tachycardia, and increased pulmonary artery pressure (PAP). Another major periprocedural complication is pulmonary artery dissection. After the procedure, lung injury can develop due to vascular injury or reperfusion. It is characterised by radiographic opacity with or without haemoptysis and with or without hypoxaemia. The treatment of BPA-related lung injury depends on the severity: in case of mild lung injury, no treatment is needed; for moderate injury, supplemental oxygen; and for severe injury, ventilation is recommended. These topics were discussed during the sixth World Symposium on Pulmonary Hypertension (WSPH), which took place in February/March 2018 in Nice, France.
Outstanding issues about BPA
There are some main outstanding issues in non-operable CTEPH patients. First, there has not been an RCT comparing the safety and efficacy of medical therapy and BPA in newly diagnosed patients with non-operable CTEPH. The currently ongoing RACE study will compare riociguat and BPA in patients with non-operable CTEPH. Furthermore, it is unclear which impact medical therapy prior to BPA has on the safety and efficacy of BPA. Finally, the complementary actions and improvement in pulmonary haemodynamics and decreased risk of BPA-associated complications are unclear.
- Galiè N, et al. Eur Heart J. 2016;37:67-119.
- Mizoguchi H et al. Circ Cardiovasc Interv. 2012;5:748-55.
- Aoki T et al. Eur Heart J. 2017;38:3152-3159.
- Olsson KM et al. Eur Respir J. 2017;49(6).
- Ogawa A, et al. Circ J. 2018;82:1222-1230.
Posted on
Previous Article
« Macrolide antibiotics and trial with azithromycin Next Article
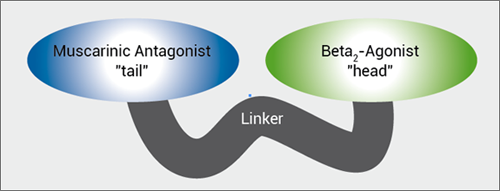
MABA, and novel LAMA »
« Macrolide antibiotics and trial with azithromycin Next Article
MABA, and novel LAMA »
Table of Contents: ERS 2018
Featured articles
Letter from The Editor
[Long Read] Current Look on Asthma
COPD: Triple Therapy, MABA and Antibiotics
Landmark triple therapy trials
ICS: to use or not to use?
MABA, and novel LAMA
Macrolide antibiotics and trial with azithromycin
Current Look on Asthma
[Long Read] Current Look on Asthma
Endoscopic Solutions
Endoscopic treatment of emphysema
Endoscopic treatment of asthma
Endoscopic treatment of chronic bronchitis
PAH
Balloon pulmonary angioplasty for CTEPH
New therapeutic targets: moving form pre-clinical data to phase 2 studies
IPF
Gastroesophageal reflux, IPF and lessons learned
Oncology
ALK inhibition, guidelines, liquid biopsies, and immunotherapy
Brain metastases, lung cancer and interstitial lung disease
Related Articles
November 7, 2018
MABA, and novel LAMA
November 7, 2018
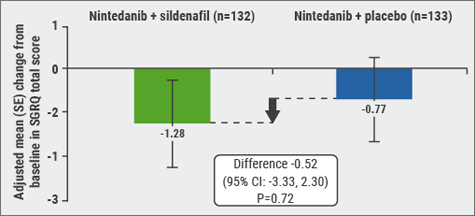
Nintedanib and sildenafil

© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

