“With respect to the pathogenesis of brain metastases, we should be aware of the blood-brain barrier [16]. In its function as security control, blocking potentially toxic substances from entering the brain, it puts a limitation on which drugs can be used.” The formation of brain metastases is based on the ‘seed and soil’ concept, so an interaction between the brain tissue and tumour cells. Multiple pathways are involved in this process. The ALK, EGFR, and VEGF pathways stimulate the proliferation, cell invasion, and angiogenesis of tumour cells, respectively [17].
Multimodal management of brain metastases
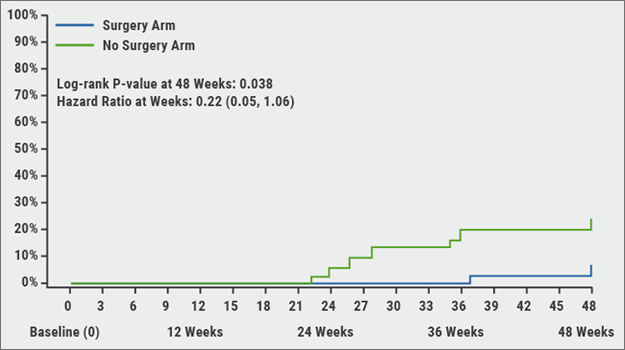
The possibility of surgical resection of brain metastases was studied in the early nineties of the previous century. “Some publications showed that surgical resection in addition to whole brain radiotherapy could improve survival”, stated Dr Blum. “Later on, it was shown that surgical resection alone led to a higher recurrence rate.” In 2016, the results of the QUARTZ trial, evaluating dexamethasone plus best supportive care with or without whole brain radiotherapy, showed a similar median overall survival between both groups (overall survival 9.2 vs 8.5 weeks, respectively; HR 1.06; P=0.8084). The same was true for the quality of life outcomes [18]. “But, a frequently suggested point of critique about this trial is that it included very sick patients with advanced disease who were unsuitable for stereotactic radiotherapy.”
Finally, Dr Blum mentioned the developments in the field of systemic treatment of brain metastases. “What is really thrilling nowadays, are the targeted therapies. We currently have some data with respect to the effect on brain metastases, although in small patient groups. EGFR-targeted treatments showed quite high response rates [19] and an improved PFS and overall survival [20]. “We are all awaiting the data of osimertinib in the treatment of brain metastases. And for ALK-targeted treatments, we have comparable promising figures” [21].
Lung cancer and interstitial lung disease
Prof. Jacques Cadranel (Constitutive Center on Rare Pulmonary Diseases, Paris, France) stated that there is an association between different forms of interstitial lung disease (ILD) [22], especially interstitial lung fibrosis (IPF), and the risk of lung cancer. Both conditions have common risk factors, such as higher age and smoking [23]. Lung cancer in IPF patients mainly presents in the lower lobe, usually in a lobe with fibrosis. The volume double time of a lung cancer nodule is usually ≤90 days [24]. The treatment of locally advanced NSCLC should be a combination of radiation therapy and chemotherapy. However, there are very few studies evaluating the efficacy and toxicity of conventional radiation therapy in patients with ILD-associated lung cancer. In total, 27-31% of radiation pneumonitis in IPF and 54% of fatal radiation pneumonitis were from patients with pre-treatment ILD [25]. According to Prof. Cadranel, conventional radiation therapy should not be used in lung cancer patients with IPF [26].
- Kromer C, et al. J Neurooncol. 2017;134:55-64.
- Waqar SN, et al. Clin Lung Cancer. 2018;19:e373-e379.
- Yawn BP, et al. Minn Med. 2003;86:32-7.
- Takei H, et al. Brain Tumor Pathol. 2016;33:1-12.
- Ciminera AK, et al. Clin Exp Metastasis. 2017;34:401-410.
- Ni W, et al. Cancer Med. 2018;7:3820-3833.
- Mulvenna P, et al. Lancet. 2016;388:2004-2014.
- Ulahannan D, et al. Ann Oncol. 2017;28:2923-2931.
- Wang X, et al. Transl Oncol. 2018;11:1119-1127.
- Waqar SN, et al. Hematol Oncol Clin North Am. 2017;31:157-176.
- Travis WD, et al. Am J Respir Crit Care Med. 2013;188:733-48.
- Meiners S, et al. Eur Respir J. 2015;45:807-27.
- Tzouvelekis A, et al. Lancet Respir Med. 2018;6:86-88.
- Vogelius IR, Bentzen SM. Acta Oncol. 2012;51:975-83.
- Vansteenkiste J, et al. Ann Oncol. 2013;24 Suppl 6:vi89-98.
Posted on
Previous Article
« Gastroesophageal reflux, IPF and lessons learned Next Article
Endoscopic treatment of chronic bronchitis »
« Gastroesophageal reflux, IPF and lessons learned Next Article
Endoscopic treatment of chronic bronchitis »
Related Articles

November 7, 2018
Balloon pulmonary angioplasty for CTEPH
November 7, 2018
Gastroesophageal reflux, IPF and lessons learned
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

