There is a possible relationship between abnormal gastroesophageal reflux (GER) and the development or progression of IPF, and risk of acute exacerbation. The hypothesis is that, in a genetically predisposed person, recurrent injury to epithelium caused by micro-aspiration of contents of gastric juice (refluxate), leads to alveolar damage and pulmonary fibrosis and ultimately to the manifestation of (pre-existing) IPF. “GER has a high prevalence in this patient population, so we need to prevent micro-aspiration”, concluded Prof. Raghu based on this concept. Retrospective data showed that Nissen fundoplication, a laparoscopic surgical procedure to treat gastroesophageal reflux disease (GERD), improves survival. Prof. Raghu and others undertook a multicentre, randomised, controlled phase 2 trial, the WRAP-IPF study. The results were published recently in The Lancet Respiratory Medicine [13]. The WRAP-IPF trial determined whether treatment of abnormal acid GER with laparoscopic anti-reflux surgery reduced the rate of disease progression of IPF. Patients with IPF, abnormal acid GER (DeMeester score of ≥14.7), and preserved FVC were recruited from 6 academic centres in the USA. Concomitant therapy with nintedanib and pirfenidone was allowed. Of the 72 originally screened patients, 58 patients randomly received surgery or no surgery. A total of 27 patients in the surgery group and 20 patients in the no surgery group had an FVC measurement at 48 weeks (P=0.041). The primary endpoint was change in FVC from randomisation to week 48. Intention-to-treat analysis (adjusted for baseline anti-fibrotic use) demonstrated an adjusted rate of change in FVC over 48 weeks was:
- -0.05 L (95% CI -0.15 to 0.05) in the surgery group and
- -0.13 L (95% CI -0.23 to -0.02) in the non-surgery group (P=0.28).
Acute exacerbation, respiratory-related hospitalisation, and death was less common in the surgery group, but the difference was not statistically significant. The time to composite endpoint was significantly different (see Figure).
Figure: Kaplan-Meier estimates of time to the composite endpoint of 10% decline in FVC or death in the WRAP-IPF study
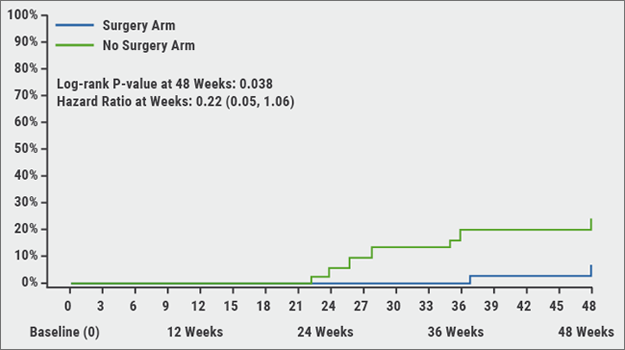
In conclusion, the WRAP-IPF study showed that laparoscopic anti-reflux surgery in patients with IPF and abnormal acid GER is safe and well tolerated. Abnormal acid GER was normalised after surgery in all patients. There was no statistically significant impact of laparoscopic anti-reflux surgery on FVC decline. However, according to Prof. Raghu, secondary endpoints are encouraging and warrant a large, well powered, randomised controlled study of anti-reflux surgery in this select population of patients with abnormal acid GER.
Lessons learned & treatment guidelines
Based on the published reports of clinical trials since 1991, Prof. Raghu summed up some lessons learned. “First, we have learned that what works or worked at the bench and is biologically plausible does not necessarily work at the bedside”, he stated. “Standard physiological/clinical assessment of disease progression is still the current standard of assessment of treatment response.”
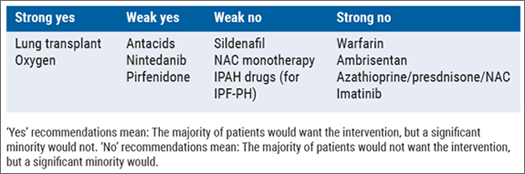
With respect to the treatment of IPF, he mentioned the following take-away: “Preventive measures might minimise risks for micro-aspiration. Cellular, molecular, and genetic biomarkers are being considered to stratify treatment in new clinical trials. Recent pharmacogenomic data from a subgroup of patients participating in the PANTHER trial is encouraging for the use of NAC in some patients, based on a specific genotype [14].” In the IPF treatment guidelines, there are currently no pharmaceutical treatments with a “strong yes” recommendation (see Table). “This void needs to be filled in, hopefully based on the finding of new clinical trials.”
Table: Treatment recommendations in the 2015 international guidelines for the treatment of IPF [5]
- Raghu G, et al. Am J Respir Crit Care Med. 2015;192:e3-19.
- Raghu G, et al. Lancet Respir Med. 2018;6:707-714.
- Oldham JM, et al. Am J Respir Crit Care Med. 2015;192:1475-82.
Posted on
Previous Article
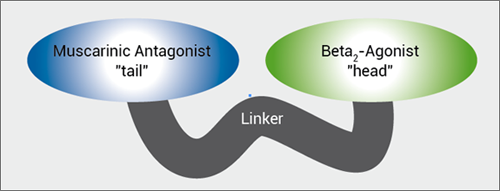
« MABA, and novel LAMA Next Article
Brain metastases, lung cancer and interstitial lung disease »
« MABA, and novel LAMA Next Article
Brain metastases, lung cancer and interstitial lung disease »
Table of Contents: ERS 2018
Featured articles
Letter from The Editor
[Long Read] Current Look on Asthma
COPD: Triple Therapy, MABA and Antibiotics
Landmark triple therapy trials
ICS: to use or not to use?
MABA, and novel LAMA
Macrolide antibiotics and trial with azithromycin
Current Look on Asthma
[Long Read] Current Look on Asthma
Endoscopic Solutions
Endoscopic treatment of emphysema
Endoscopic treatment of asthma
Endoscopic treatment of chronic bronchitis
PAH
Balloon pulmonary angioplasty for CTEPH
New therapeutic targets: moving form pre-clinical data to phase 2 studies
IPF
Gastroesophageal reflux, IPF and lessons learned
Oncology
ALK inhibition, guidelines, liquid biopsies, and immunotherapy
Brain metastases, lung cancer and interstitial lung disease
Related Articles
November 7, 2018
Landmark triple therapy trials
November 7, 2018
IPF introduction and Pentraxin-2
November 7, 2018
MABA, and novel LAMA
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

