https://doi.org/10.55788/d540f471
Fibromyalgia, characterised by widespread pain, fatigue, sleep disturbances, and functional symptoms, has a worldwide prevalence of 2–3% [1]. However, a meta-analysis published previously showed that the prevalence of fibromyalgia in the general population is significantly lower than in populations with certain diseases and can be as high as 12.9% in patients with IBD [1]. Information on the prevalence and the impact of fibromyalgia in patients with IBD is limited. To address this knowledge gap, Dr Laura Guida (Luigi Sacco University Hospital, Italy) and her team performed a study on consecutive patients attending 2 IBD hospital units from August to November 2021 [2]. Excluded were patients with severe disease activity (assessed by Crohn’s disease activity index [CDAI] and Mayo score for ulcerative colitis [UC]) or those with other concomitant chronic diseases. Clinical and demographic data and patient-reported outcomes (PROs) were collected using the IBD Questionnaire (IBD-Q), Depression Anxiety Stress Scale-21 (DASS-21), Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F), and Pittsburgh Sleep Quality Index (PSQI). An expert rheumatologist diagnosed fibromyalgia according to the 2011 ACR classification criteria.
Among the 196 IBD patients enrolled in the study, 105 (53.6%) had Crohn’s disease (CD), and the rest had UC. The overall prevalence of fibromyalgia in the IBD cohort was 8.7%, with 7.6% in the CD group and 9.9% in the UC group. As expected, the prevalence was higher in women (11.6%) than in men (6.3%). No significant demographic (i.e. gender, age) or clinical (i.e. body mass index, C-reactive protein, disease activity, ongoing treatment modality) differences were found between the groups with and without fibromyalgia as comorbidity.
As assessed by IBD-Q, the quality-of-life in IBD patients with fibromyalgia was significantly lower than in those who did not have fibromyalgia (P<0.001). Furthermore, they experienced significantly worse symptoms (i.e. depression, anxiety, stress, chronic fatigue, and discomfort) than patients without fibromyalgia (P<0.001; see Table).
Table: High prevalence of depression, anxiety, and stress in patients with inflammatory bowel disease and fibromyalgia [1]
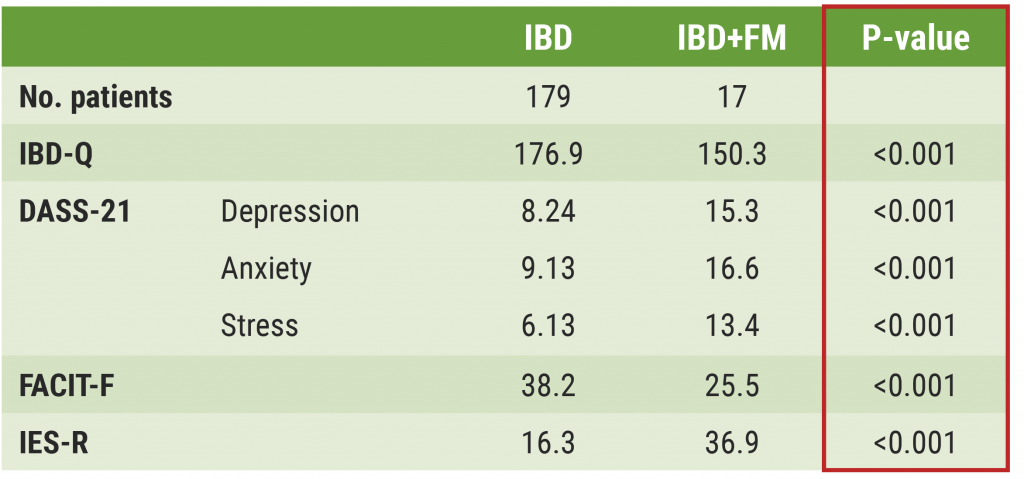
IBD, inflammatory bowel disease; FM, fibromyalgia; IBD-Q, inflammatory bowel disease Questionnaire; DASS-21, Depression Anxiety Stress Scale-21; FACIT-F, Functional Assessment of Chronic Illness Therapy-Fatigue; IES-R, Impact of Event Scale-Revised.
Moreover, multivariate analysis showed that disease activity (CDAI; P=0.025), chronic fatigue (FACIT-F; P=0.006), and sleep disturbances (PSQI; P=0.044) have a significant influence on the quality-of-life of CD patients. In contrast, disease severity (Mayo score; P=0.012) was the only independent variable that positively correlated with quality-of-life in UC patients.
In conclusion, Dr Guida emphasised that the presence of fibromyalgia in IBD can considerably impact the quality-of-life, especially by causing depression, anxiety, stress, chronic fatigue, sleep disturbances, and discomfort.
- GuidaL, et al. Prevalence and impact of fibromyalgia in patients with inflammatory bowel disease. POS0023, EULAR 2022 Congress, 1-4 June, Copenhagen, Denmark.
- Heidari F, et al. Rheumatol Int. 2017;37:1527–1539.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Inhibition of Bruton’s tyrosine kinase: a new way of approaching SLE? Next Article
Alarmingly low activity in patients with non-inflammatory and inflammatory rheumatic disease »
« Inhibition of Bruton’s tyrosine kinase: a new way of approaching SLE? Next Article
Alarmingly low activity in patients with non-inflammatory and inflammatory rheumatic disease »
Table of Contents: EULAR 2022
Featured articles
Late-Breaking Oral Abstracts
TYK2 inhibition: the future of treating lupus erythematosus?
Psoriatic arthritis: significant improvement with bimekizumab
Baricitinib could open the door to oral treatment for juvenile idiopathic arthritis
Sarilumab for polymyalgia rheumatica led to sustained remission and fewer flares
Spotlight on Rheumatoid Arthritis
Comorbid depression comes with a profoundly higher mortality risk in RA
Preventive treatment with methotrexate benefits pre-RA patients with arthralgia
Risk factors for dementia in RA patients discovered
VTE in global registry data more common in JAK inhibitor-treated RA patients
Spondyloarthropathies – Novel Developments
How to treat enthesitis in 2022
Baseline cardiovascular risk linked to higher rates of MACE in PsA and PsO patients receiving tofacitinib
Treat-to-target dose reduction effective in spondyloarthritis
A novel oral treatment possibility for non-radiographic axSpA on the horizon
Many RA and PsA patients have problems with their sex life
What Is Hot in Osteoarthritis?
New treatments in osteoarthritis
OA associated with alcohol and drug abuse
Body mass index increase associated with structural changes in knee OA
What Is New in Lupus and Scleroderma
Inhibition of Bruton’s tyrosine kinase: a new way of approaching SLE?
Pregnancies in SLE: many complications for mothers and their unborn children
Lupus nephritis: Efficient treatment may reduce the risk of kidney disease advancement
Antifibrotic therapy with nintedanib is beneficial for patients with negative prognostic factors
Best of the Posters
Alarmingly low activity in patients with non-inflammatory and inflammatory rheumatic disease
High prevalence of fibromyalgia in patients with inflammatory bowel disease
Related Articles

March 8, 2022
ECCO 2022 Highlights Podcast
December 7, 2023
Obefazimod takes the spotlight as promising UC treatment
December 1, 2022
Sustained maintenance results with upadacitinib in UC
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

