https://doi.org/10.55788/eba5695d
Based on 6 simulation models of the Cancer Intervention and Surveillance Modelling Network (CISNET), Prof. Jennifer Caswell-Jin (Stanford University, CA, USA) and co-investigators aimed to assess whether advances in metastatic therapies have resulted in a reduced population-level breast-cancer mortality in the last 2 decades [1]. The contribution of screening and early-stage therapy on mortality reduction in patients with breast cancer was assessed in previous research [2].
In 2019, the combination of screening, early-stage treatment, and metastatic treatment resulted in a reduced overall mortality of patients with breast cancer of 58% compared with no intervention. The largest reduction was observed in the ER-positive/HER2-positive subpopulation (71%), whereas the least progress was made in patients with triple-negative breast cancer (40%). In addition, the reduction in mortality rates in patients with ER-negative/HER2-positive or ER-positive/HER2-negative were 61% and 59%, respectively.
According to Prof. Caswell-Jin, the relative contribution of metastatic therapies to reduced mortality varies over time, depending on the distribution of transitioning therapies. When metastatic therapies are transitioned to early-stage therapies, the relative contribution of metastatic therapies to the improvement in overall survival is decreased. In 2019, 19% of the overall mortality reduction was attributed to metastatic therapies. Furthermore, metastatic therapies have improved the median overall survival of patients with ER-positive/HER2-negative breast cancer after distant recurrence from 2.0 to 3.5 years in the last 2 decades. Correspondingly, the median overall survival after distant recurrence increased from 1.2 to 1.8 years in ER-negative/HER2-negative patients, from 2.3 to 4.8 years in ER-positive/HER2-positive patients, and from 2.2 to 3.9 years in ER-negative/HER2-positive patients (see Figure).
Figure: Median survival after distant recurrence for HER2-positive (up) and HER-negative (down) subtypes [1]

“Steady introduction of new metastatic treatments in the last 2 decades has been essential to the observed mortality reduction in patients with breast cancer,” concluded Prof. Caswell-Jin.
- Caswell-Jin J, et al. Contributions of screening, early-stage treatment, and metastatic treatment to breast cancer mortality reduction by molecular subtype in U.S. women, 2000-2017. Abstract 1008, ASCO 2022 Annual Meeting, 3‒7 June, Chicago, IL, USA.
- Plevritis SK, et al. JAMA. 2018;319(2):154–164.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Radiotherapy may be omitted in breast cancer patients Next Article
Analysis by residual cancer burden further clarifies effect of pembrolizumab »
« Radiotherapy may be omitted in breast cancer patients Next Article
Analysis by residual cancer burden further clarifies effect of pembrolizumab »
Table of Contents: ASCO 2022
Featured articles
Breast Cancer
Sacituzumab govitecan meets primary endpoint
Shaky OS results of palbociclib in ER-positive/HER2-negative breast cancer
Practice-changing results of T-DXd in HER2-low breast cancer
SET2,3 to inform on chemotherapy decisions in ER-positive breast cancer
Metastasis-directed therapy fails in oligometastatic breast cancer
Analysis by residual cancer burden further clarifies effect of pembrolizumab
Contribution of metastatic therapies on mortality reduction in breast cancer
Radiotherapy may be omitted in breast cancer patients
Promising data for ribociclib after progression on ET plus CDK4/6 inhibitors in HR-positive/HER2-negative metastatic breast cancer
7-gene biosignature: Benefits of endocrine therapy and radiotherapy in breast cancer risk groups
Lung Cancer
Additional tiragolumab does not help patients with untreated small cell lung cancer
Success for serplulimab plus chemotherapy in small cell lung cancer
Adagrasib safe and clinically active in non-small cell lung cancer
Long-term benefits of combined immunotherapy over chemotherapy in non-small cell lung cancer
Effect of KRAS mutations and PD-L1 expression on therapy response in non-small cell lung cancer
Melanoma
First results on distant metastasis-free survival in stage II melanoma
Higher response rates for concurrent triple therapy versus sequential therapy in melanoma
Genitourinary Cancers
Exploratory treatment options fail in ccRCC
Adjuvant everolimus did not benefit high-risk renal cell carcinoma
Cabozantinib fails as first-line maintenance therapy in urothelial cancer
177Lu-PSMA-617 is a valid treatment option for PSMA-positive mCRPC
Enzalutamide performs well in metastatic hormone-sensitive prostate cancer
Haematologic Malignancies
Autologous stem cell transplantation plus RVd improves PFS in multiple myeloma
Novel first-line treatment option for mantle cell lymphoma
Promising results for novel CAR-T therapy in relapsed/refractory multiple myeloma
Gastrointestinal Cancers
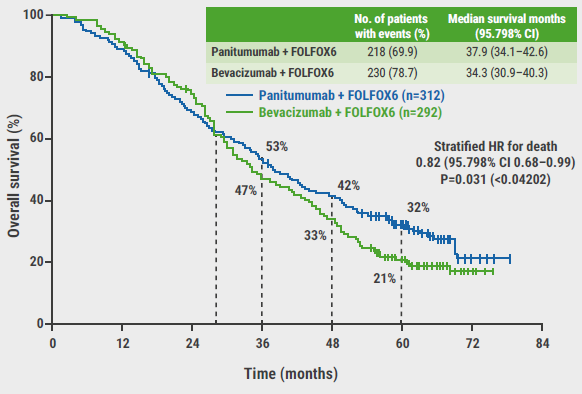
Panitumumab beats bevacizumab in RAS wildtype left-sided metastatic colorectal cancer
Spectacular results for dostarlimab in mismatch repair deficient rectal cancer
Triplet chemotherapy beats doublet chemotherapy in colorectal cancer liver metastases
To resect or not to resect primary tumours in stage IV colon cancer?
Novel treatment option for KRAS wildtype pancreatic cancer
Gynaecological Cancers
Primary results of rucaparib in ovarian cancer
Trabectedin not superior to chemotherapy in recurrent epithelial ovarian cancer
Encouraging results of relacorilant in ovarian cancer
Miscellaneous Topics
Bacterial decolonisation effective against radiation dermatitis
New standard-of-care for cisplatin-ineligible locally advanced head and neck squamous cell carcinoma
Ifosfamide is likely to be the go-to therapy in recurrent Ewing sarcoma
Dabrafenib plus trametinib candidates for standard-of-care in BRAF V600-mutated paediatric low-grade glioma
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com