Dr George Goshua (Yale University, USA) presented the data, which followed up on the observation in SARS-CoV-2-infected individuals of a marked increase of clinical thrombotic and microvascular complications, referred to as COVID-19-associated coagulopathy (CAC) [1].
Despite thromboprophylaxis, CAC is still highly prevalent among hospitalised patients, with venous thromboembolism detected in 17% to 69% of patients. Furthermore, autopsy findings have shown microvascular thrombosis in as many as 87% of patients. The aetiology is unknown.
Dr Goshua and colleagues assessed endothelial cell damage, platelet activation, and haemostatic and fibrinolytic cascade effects of CAC in stable and critically ill patients hospitalised with COVID-19 (n=68). Of those, 48 were in the ICU (on mechanical ventilation) and 20 were outside the ICU (on supplemental oxygen), and an additional cohort of 13 non-hospitalised, asymptomatic patients were used as a comparator reference control group. There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
As anticipated, D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations were increased, but levels were significantly higher (P<0.001) among the ICU patients. Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (α 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as plasminogen activation inhibitor 1 (PAI-1) was high in both ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%). Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (mean 565 ± 199% in ICU patients vs 278 ± 133% in non-ICU patients; P<0.0001) in the ICU cohort. Soluble P-selectin was also higher in the ICU patients (15.9 ± 4.8 ng/mL vs 11.2 ± 3.1 ng/mL; P=0.0014). Mortality significantly correlated with Von Willebrand factor antigen (R=0.38; P=0.0022) and soluble thrombomodulin (R=0.38; P=0.0078) in all patients. Furthermore, soluble thrombomodulin concentrations >3.26 ng/mL were associated with lower rates of hospital discharge (P=0.0050) and lower likelihood of survival (HR 5.9; 95% CI 1.9-18.4; P=0.0087).
In conclusion, markers of endothelial damage suggest pathophysiological aetiology and can be used to predict disease outcomes. Early identification of endotheliopathy, with consequent management, may improve outcomes in COVID-19.
- Goshua G, et al. Endotheliopathy is essential in COVID-19 associated coagulopathy. EHA25 Virtual, 11-21 June 2020, Abstract LB2605.
Posted on
Previous Article
« Paroxysmal nocturnal haemoglobinuria treatment with pegcetacoplan Next Article
Carfilzomib: no PFS benefit for multiple myeloma »
« Paroxysmal nocturnal haemoglobinuria treatment with pegcetacoplan Next Article
Carfilzomib: no PFS benefit for multiple myeloma »
Table of Contents: EHA 2020
Featured articles
Myeloid
VIALE-A: newly diagnosed chemo-ineligible AML
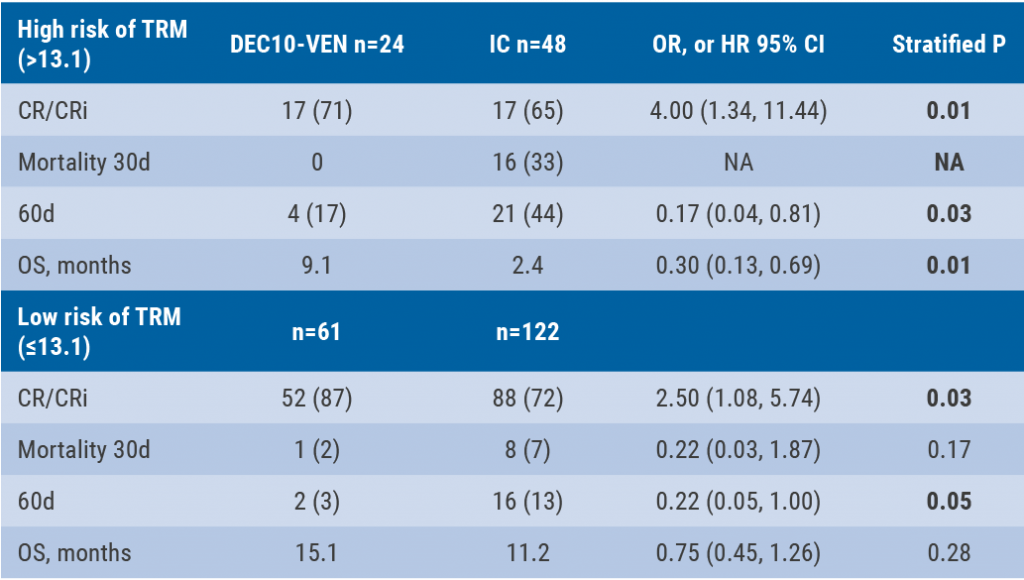
DEC10-VEN superior to intensive chemotherapy in high-risk AML
Magrolimab plus azacitidine: good ORR in MDS/AML
Asciminib monotherapy in Ph+ CML: major molecular responses
CML TKI interruption: Swedish registry results
Patients with lower-risk MDS benefit from imetelstat
Better outcomes adding enasidenib to azacitidine in mIDH2-AML
Lymphoid
PET-stratification can omit radiotherapy in early-stage unfavourable Hodgkin lymphoma
Pembrolizumab improves PFS for relapsed/refractory Hodgkin lymphoma
Promising first-in-human trial of epcoritamab in B-NHL
Two trials: acalabrutinib in CLL
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia
Deep responses in R/R CLL with venetoclax monotherapy
MRD assessment post-CAR-T predicts ALL allo-HSCT bridging
Plasma Cell Dyscrasias
Daratumumab for light-chain amyloidosis
Isatuximab triplet improves PFS in R/R MM
Initial results from CAR-T cell therapy in MM: KarMMa
Graft-Versus-Host Disease
GRAVITAS-301: improved complete aGVDH response
Ruxolitinib improves steroid-refractory aGVHD across subtypes
Benign Haematology
Paroxysmal nocturnal haemoglobinuria treatment with pegcetacoplan
Mitapivat, a pyruvate kinase-R activator, in SCD is safe with early efficacy results
SCD LentiGlobin gene therapy: new data on VOC and ACS
Paediatric Haematology
Venetoclax + navitoclax promising for R/R ALL or LL
Nivolumab/brentuximab vedotin in R/R HL: good CMR rates
Bench-to-Bedside Science from the Presidential Symposium
Microbiome predicts B-ALL predisposition
Netrin-1 regulates haematopoietic stem cells
Unrecognised role of iron in neutrophil differentiation
Related Articles
September 9, 2020
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia
September 9, 2020
DEC10-VEN superior to intensive chemotherapy in high-risk AML
September 9, 2020
Daratumumab for light-chain amyloidosis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

