https://doi.org/10.55788/1b96b97e
Dr Julie Kanter (University of Alabama, USA) provided new results on the largest cohort of the study, Group C, in which stem cells were extracted from the peripheral blood of patients by plerixafor mobilisation and apheresis, instead of bone marrow, with an altered protocol for gene therapy transduction with LentiGlobin gene therapy [1]. LentiGlobin therapy transduces autologous CD34+ cells with the BB305 lentiviral vector, encoding a human β-globin gene with the anti-sickling T87Q mutation (βA-T87Q). Patients underwent myeloablation with busulfan before infusion with the transduced cells and were then monitored for engraftment, safety, and efficacy.
In Group C of HGB-206, 25 SCD patients were treated with LentiGlobin, with follow-up up to 24.8 months (median 12.1 months); 18 patients had been followed for at least 6 months.
Median levels of gene-therapy-derived βA-T87Q contributed to >40% of total haemoglobin. At last visit, total haemoglobin ranged from 9.6-16.2 g/dL, and βA-T87Q levels ranged from 2.7-9.4 g/dL. At month 6, the production of βA-T87Q was associated with a reduction in the proportion of sickle cell haemoglobin (HbS) in total haemoglobin.
All patients in Group C were able to stop regular blood transfusions and remain off transfusions at 3 months post-treatment. There was a 99.5% mean reduction in annualised rate of VOCs and ACS among the 14 patients who had at least 6 months of follow-up and a history of VOCs or ACS, defined as 4 or more VOCs or ACS events in the 2 years prior to treatment (median was 8 events). There were no reports of serious VOCs or ACS up to 24 months post-treatment in patients.
Patients treated with LentiGlobin for SCD demonstrated improvement in key markers of haemolysis, as well. By month 6 post-treatment, reticulocyte counts, lactate dehydrogenase, and total bilirubin normalised compared with pre-treatment. In 9 patients who had at least 6 months of follow-up, the average proportion of red blood cells positive for βA-T87Q was greater than 70%, and on average more than 85% of red blood cells contained βA-T87Q at 18 months post-treatment, suggesting near-complete pancellularity of βA-T87Q distribution.
At data cut-off in March 2020, the safety data from all patients in HGB-206 are generally reflective of SCD and the known side effects of haematopoietic stem cell collection, including myeloablative conditioning. There were no serious adverse events related to LentiGlobin for SCD, and the non-serious related adverse events were mild-to-moderate and self-limited. One patient with a history of frequent pre-treatment VOCs, pulmonary and systemic hypertension, venous thrombosis, obesity, sleep apnoea, and asthma had complete resolution of VOCs following treatment, but suffered sudden death 20 months after treatment with LentiGlobin for SCD. The patient's autopsy revealed cardiac enlargement and fibrosis, and concluded the cause of death was cardiovascular, with contributions from SCD and asthma. An independent monitoring committee agreed this death was unlikely related to LentiGlobin for SCD gene therapy.
In conclusion, LentiGlobin gene therapy not only appears to be safe, with stable transduction levels which result in stable supplementation of HbS with βA-T87Q, biological markers of SCD normalise, resulting in transfusion-independence and resolution of VOCs and ASC events.
- Kanter J, et al. Outcomes in patients treated with lentiglobin for sickle cell disease (SCD) gene therapy: updated results from the phase 1/2 HGB-206 GROUP C study. EHA25 Virtual, 11-21 June 2020, Abstract S282.
Posted on
Previous Article
« Venetoclax + navitoclax promising for R/R ALL or LL Next Article
Toripalimab plus axitinib effective in metastatic mucosal melanoma »
« Venetoclax + navitoclax promising for R/R ALL or LL Next Article
Toripalimab plus axitinib effective in metastatic mucosal melanoma »
Table of Contents: EHA 2020
Featured articles
Myeloid
VIALE-A: newly diagnosed chemo-ineligible AML
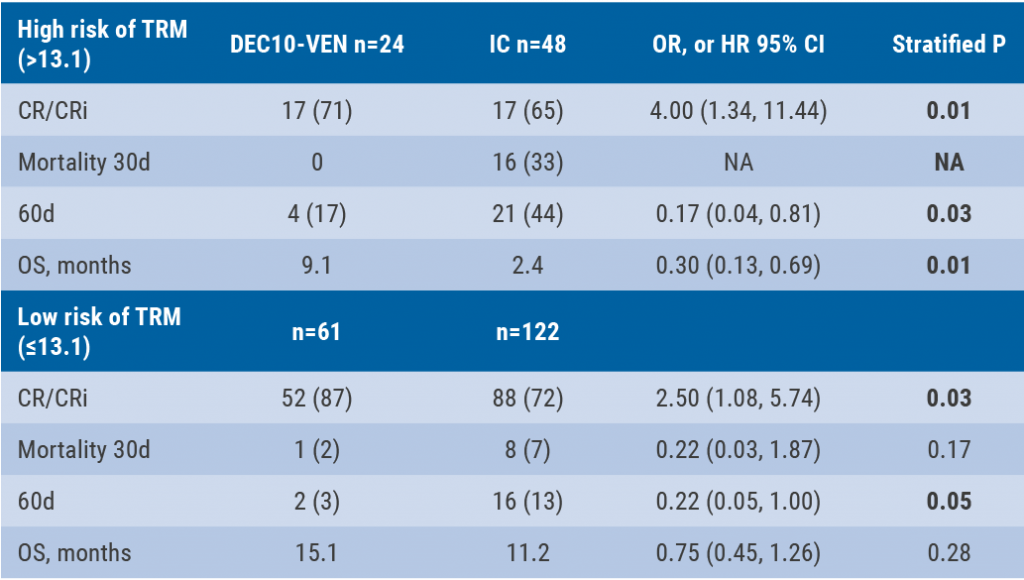
DEC10-VEN superior to intensive chemotherapy in high-risk AML
Magrolimab plus azacitidine: good ORR in MDS/AML
Asciminib monotherapy in Ph+ CML: major molecular responses
CML TKI interruption: Swedish registry results
Patients with lower-risk MDS benefit from imetelstat
Better outcomes adding enasidenib to azacitidine in mIDH2-AML
Lymphoid
PET-stratification can omit radiotherapy in early-stage unfavourable Hodgkin lymphoma
Pembrolizumab improves PFS for relapsed/refractory Hodgkin lymphoma
Promising first-in-human trial of epcoritamab in B-NHL
Two trials: acalabrutinib in CLL
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia
Deep responses in R/R CLL with venetoclax monotherapy
MRD assessment post-CAR-T predicts ALL allo-HSCT bridging
Plasma Cell Dyscrasias
Daratumumab for light-chain amyloidosis
Isatuximab triplet improves PFS in R/R MM
Initial results from CAR-T cell therapy in MM: KarMMa
Graft-Versus-Host Disease
GRAVITAS-301: improved complete aGVDH response
Ruxolitinib improves steroid-refractory aGVHD across subtypes
Benign Haematology
Paroxysmal nocturnal haemoglobinuria treatment with pegcetacoplan
Mitapivat, a pyruvate kinase-R activator, in SCD is safe with early efficacy results
SCD LentiGlobin gene therapy: new data on VOC and ACS
Paediatric Haematology
Venetoclax + navitoclax promising for R/R ALL or LL
Nivolumab/brentuximab vedotin in R/R HL: good CMR rates
Bench-to-Bedside Science from the Presidential Symposium
Microbiome predicts B-ALL predisposition
Netrin-1 regulates haematopoietic stem cells
Unrecognised role of iron in neutrophil differentiation
Related Articles
August 28, 2020
Netrin-1 regulates haematopoietic stem cells

September 9, 2020
EHA25 Highlights Podcast
September 9, 2020
DEC10-VEN superior to intensive chemotherapy in high-risk AML
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

