Prof. Elias Jabbour (University of Texas MS Anderson Cancer Centre, USA) presented the phase 1, multicentre, open-label, dose-escalation study [1], addressing the unmet need for new treatment options in R/R ALL and LL. The investigators hypothesised that BCL2 inhibitor venetoclax in combination with low-dose navitoclax (a BCL-XL inhibitor) could improve efficacy while minimising dose-limiting toxicities known to occur with standard-dose navitoclax monotherapy.
Patients (n=47, median age 29 years, median number of prior therapies was 4) received 400 mg venetoclax (weight-adjusted equivalent) daily, together with daily oral navitoclax at 25, 50, 100 mg for patients ≥45 kg, or 25, 50 mg for patients <45 kg. Dose-limiting toxicities were observed in 7 patients: neutropenia (25 mg); neutropenia and drug-induced liver injury (50 mg); ischaemic bowel, hyper bilirubinaemia, pancytopenia, and delayed count recovery (100 mg).
The recommended dose for phase 2 navitoclax (in combination with 400 mg venetoclax) was determined to be 50 mg for patients ≥45 kg or 25 mg for patients <45 kg. The most common grade 3/4 adverse events (AEs) were febrile neutropenia (39%), neutropenia (26%), and hypokalaemia (24%). Non-haematologic grade 3/4 treatment-emergent AEs related to venetoclax or navitoclax included vomiting (n=3), increased ALT (n=2), and sepsis (n=2). One death due to intestinal ischaemia was attributed to the study drug combination.
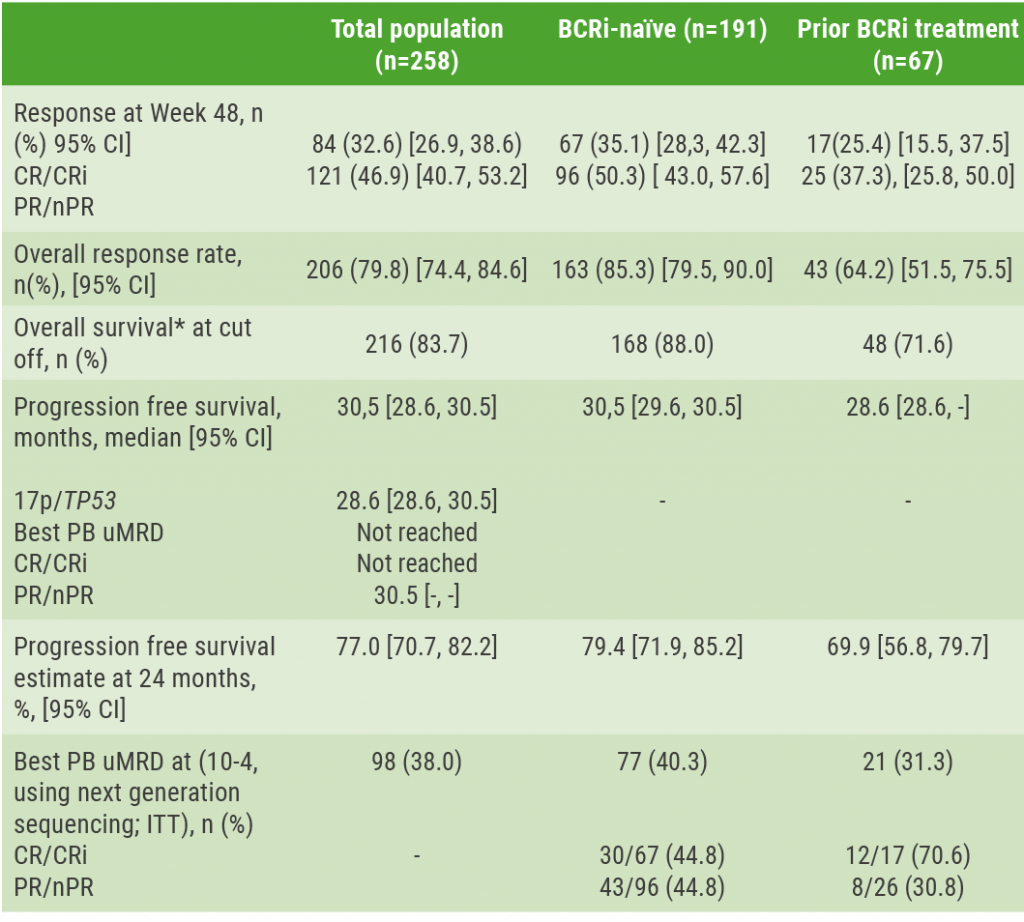
Complete response with or without incomplete haematological recovery (CR/CRi) was achieved by 25 (54%) patients with 15 (33%) achieving undetectable minimal residual disease (MRD). Median overall survival (OS) was 9.7 months for B-cell ALL patients and 6.6 months for T-cell ALL patients. A total of 11 (24%) patients went on to stem cell transplant or CAR-T. In a subgroup analysis, paediatric patients had similar results; CR/CRi was 58%, 50% had undetectable MRD, and median OS was 9.7 months. Similar CR rates were observed across additional subgroups (see Figure).
Figure: CR rate for all assessed subgroups [1]

ALL, acute lymphoblastic leukaemia; BM, bone marrow; CAR-T, chimeric antigen receptor T; CR, complete response; CR rate, CR + CRi + CRp; LL, lymphoblastic lymphoma.
*5 ALL patients had BM blasts <5% at baseline and are included in the total study population. Of these 5 patients, 4 remained CR after treatment and achieved uMRD.
In conclusion, venetoclax + navitoclax with chemotherapy is well-tolerated, and efficacy is promising in heavily pre-treated patients (including those with prior blinatumomab, inotuzumab, or CAR-T) with suggestive high rates of CR/CRi.
- Jabbour E, et al. Venetoclax and navitoclax in relapsed or refractory acute lymphoblastic leukemia and lymphoblastic lymphoma. EHA25 Virtual, 11-21 June 2020, Abstract S116.
Posted on
Previous Article
« Microbiome predicts B-ALL predisposition Next Article
SCD LentiGlobin gene therapy: new data on VOC and ACS »
« Microbiome predicts B-ALL predisposition Next Article
SCD LentiGlobin gene therapy: new data on VOC and ACS »
Table of Contents: EHA 2020
Featured articles
Myeloid
VIALE-A: newly diagnosed chemo-ineligible AML
DEC10-VEN superior to intensive chemotherapy in high-risk AML
Magrolimab plus azacitidine: good ORR in MDS/AML
Asciminib monotherapy in Ph+ CML: major molecular responses
CML TKI interruption: Swedish registry results
Patients with lower-risk MDS benefit from imetelstat
Better outcomes adding enasidenib to azacitidine in mIDH2-AML
Lymphoid
PET-stratification can omit radiotherapy in early-stage unfavourable Hodgkin lymphoma
Pembrolizumab improves PFS for relapsed/refractory Hodgkin lymphoma
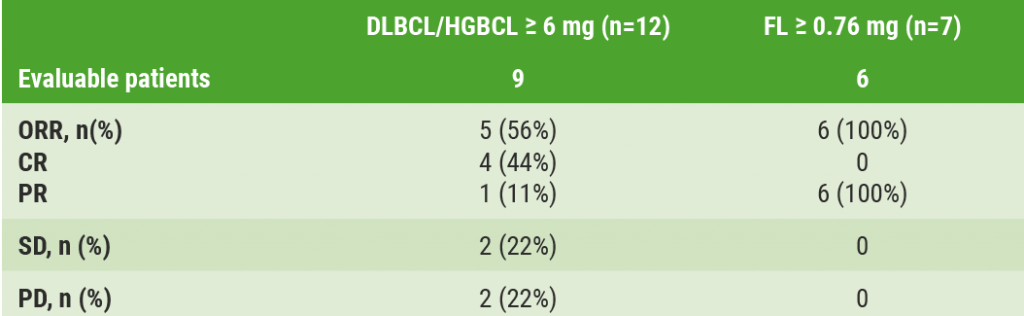
Promising first-in-human trial of epcoritamab in B-NHL
Two trials: acalabrutinib in CLL
Zanubrutinib versus ibrutinib in Waldenström macroglobulinaemia
Deep responses in R/R CLL with venetoclax monotherapy
MRD assessment post-CAR-T predicts ALL allo-HSCT bridging
Plasma Cell Dyscrasias
Daratumumab for light-chain amyloidosis
Isatuximab triplet improves PFS in R/R MM
Initial results from CAR-T cell therapy in MM: KarMMa
Graft-Versus-Host Disease
GRAVITAS-301: improved complete aGVDH response
Ruxolitinib improves steroid-refractory aGVHD across subtypes
Benign Haematology
Paroxysmal nocturnal haemoglobinuria treatment with pegcetacoplan
Mitapivat, a pyruvate kinase-R activator, in SCD is safe with early efficacy results
SCD LentiGlobin gene therapy: new data on VOC and ACS
Paediatric Haematology
Venetoclax + navitoclax promising for R/R ALL or LL
Nivolumab/brentuximab vedotin in R/R HL: good CMR rates
Bench-to-Bedside Science from the Presidential Symposium
Microbiome predicts B-ALL predisposition
Netrin-1 regulates haematopoietic stem cells
Unrecognised role of iron in neutrophil differentiation
Related Articles
August 28, 2020
Microbiome predicts B-ALL predisposition
September 9, 2020
Deep responses in R/R CLL with venetoclax monotherapy
September 9, 2020
Promising first-in-human trial of epcoritamab in B-NHL
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

